




12



The
WHO


This






12



The
WHO


This
Specialist Forum’s March issue covers a wide array of topics, from debunking myths about Parkinson’s disease to shedding light on the psychological toll of acne.
With advancements in medical research, it is extremely important to separate fact from fiction, empowering both patients and healthcare professionals with accurate information.
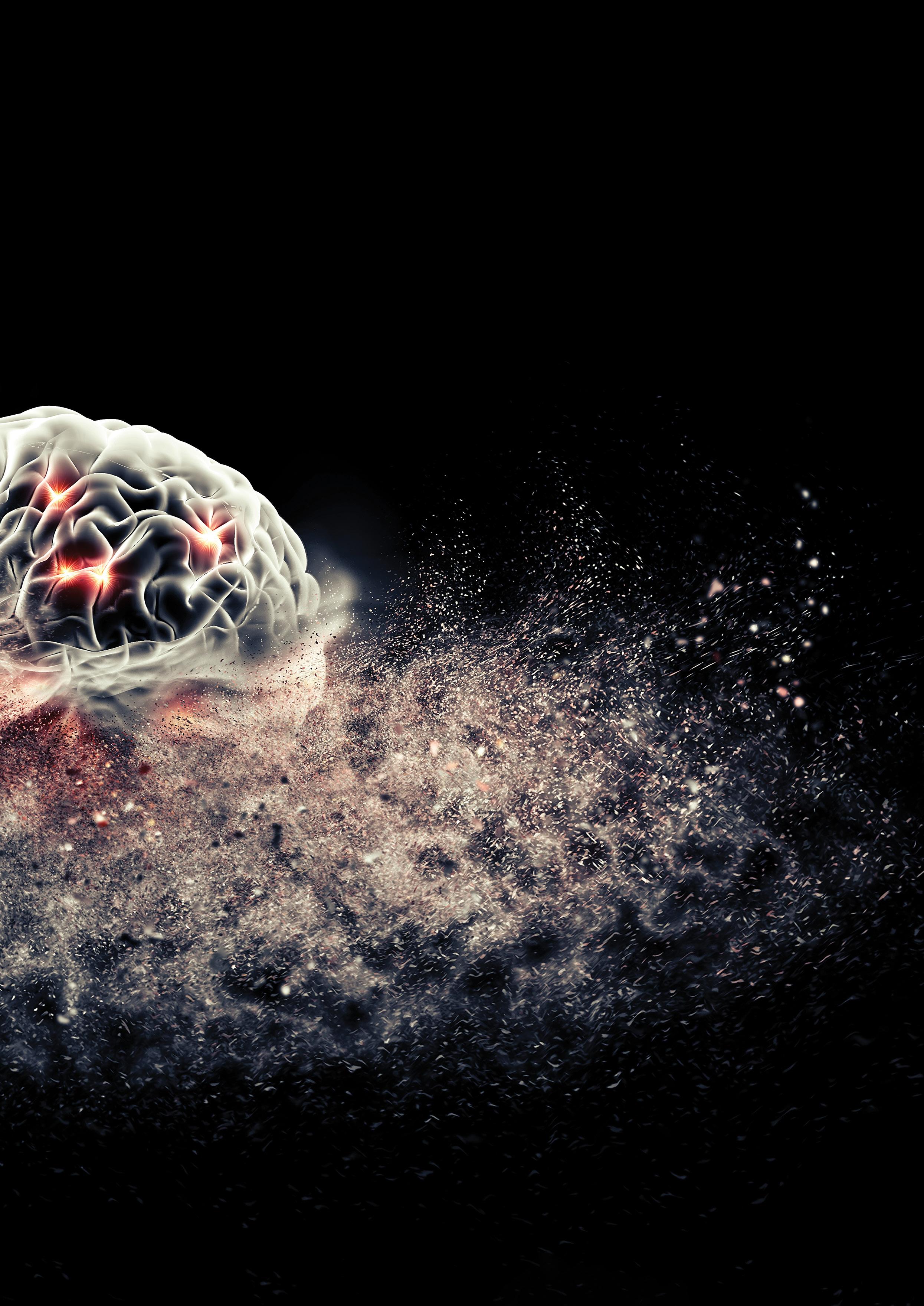
Physician burnout is a prevailing issue, and our article Physicians’ vacation woes: Burnout alert! Looks at the challenges faced by healthcare professionals when taking time off. The article sheds light on the importance of addressing burnout and emphasises the need for comprehensive strategies to ensure physicians can truly recharge during their vacations.
In the gastroenterology section, we look at the link between stress and irritable bowel syndrome (IBS). This is an online CPD article (A 2-way street: Stress and IBS), which can be accessed on Medical Academic.
In another article in the gastroenterology section, the gut-brain connection is explored. This article emphasises the impact of gut health on overall well-being. It serves as a reminder for healthcare providers to consider the gut as a crucial factor in their diagnostic and treatment approaches.
Our CPD article in the dermatology section discusses acne, which affects a large percentage of the population. Beyond the physical manifestations, the article focuses on the emotional and psychological aspects of acne, emphasising the need for a holistic approach to patient care.
EDITORIAL
EDITOR: René Bosman
René.Bosman@newmedia.co.za
SUB EDITOR: Gill Abrahams
LAYOUT & DESIGN: Allison McCallum
ADVERTISING
ADVERTISING EXECUTIVE
Charissa Piek | 063 281 1205
Charissa.Piek@newmedia.co.za
DISTRIBUTION & SUBSCRIPTIONS
Felicity Garbers
Felicity.Garbers@newmedia.co.za
PUBLISHING TEAM
GENERAL MANAGER: Dev Naidoo
GROUP ACCOUNT DIRECTOR B2B:
Johann Gerber
Johann.Gerber@newmedia.co.za
PRODUCTION MANAGER: Angela Silver
ART DIRECTOR: David Kyslinger
CONTACT
Johannesburg Office: Ground Floor, 272
Pretoria Avenue, Randburg 2194
Postal Address:
PO Box 784698, Sandton, Johannesburg, 2146
T +27(0)11 877 6111 F +27(0)11 713 9024
www.medicalacademic.co.za
PRINTING
Printed by CTP Printers
COVER PRICE
Specialist Forum per issue R80,00 VAT Incl.
ISSN: 2218-8282
Published by New Media, a division of Media24 (Pty) Ltd
Our second print CPD activity looks at the growing obesity epidemic. We take a look at innovative strategies and interventions to address this growing healthcare concern.
The rheumatology section explores the revolutionary treat to target in rheumatoid arthritis, which marks a paradigm shift in the management of patients with this debilitating disease. The third article in our CPD activity looks at the management of pain in patients living with osteoarthritis and discusses pain relief beyond analgesics.
World Glaucoma Week was from 10-16 March. Our Glaucoma: Under pressure article article stresses the importance of early detection and intervention in managing this sight-threatening condition.
Salt Awareness Week is from 20-26 May. The cardiology section shakes up the sodium debate by looking at the complex balance between sodium intake and cardiovascular health.
Hope you enjoy the read!
Regards
René Bosman

MANAGEMENT TEAM
CEO: NEW MEDIA: Aileen Lamb
COMMERCIAL DIRECTOR: Maria Tiganis
STRATEGY DIRECTOR: Andrew Nunneley
CHIEF FINANCIAL OFFICER: Venette
Malone
CEO: MEDIA24: Ishmet Davidson
HEAD OFFICE
8th floor, Media24 Centre, 40 Heerengracht, Cape Town 8001
PO Box 440, Green Point, Cape Town 8051
Tel: +27 (0)21 406 2002
www.newmedia.co.za
Disclaimer: Please take note that the products featured in this journal are available in South Africa. Products may be marketed under a different name or might not be registered in your country. For more information, contact your local representative.
All content in Specialist Forum is sourced independently and under no circumstances should articles be considered promotional unless specified with a postscript. Please note that all advertising is intended for healthcare professionals only.

Unless previously agreed in writing, Specialist Forum owns all rights to all contributions, whether image or text.
SOURCES: Shutterstock, supplied images, editorial staff.
While precautions have been taken to ensure the accuracy of its contents and information given to readers, neither the editor, publisher, or its agents can accept responsibility for damages or injury which may arise therefrom. All rights reserved. © Specialist Forum. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, photocopying, electronic, mechanical or otherwise without the prior written permission of the copyright owners.







Parkinson’s disease (PD) is the most common movement disorder. The prevalence of the disease has doubled in the last 25 years. Global figures from 2019 indicate that there were >8.5 million individuals affected by PD. In the same year, PD contributed to 5.8 million disability-adjusted life years, marking an 81% rise since 2000. Additionally, PD was associated with 329 000 deaths, reflecting an increase of over 100% since 2000.
Myth 1: PD is caused by a genetic mutation.
Fact: The precise cause of PD remains unidentified. While researchers acknowledge genetic and environmental influences, there is not a singular genetic mutation responsible for all PD cases. Although PD can be hereditary, around 90% of cases are sporadic, occurring without a family history. Additionally, possessing a mutation associated with PD does not guarantee developing the disease.
Myth 2: Parkinson’s disease (PD) is ‘only’ a condition affecting movement.
Fact: PD is commonly associated with motor symptoms like tremors and stiffness, but it involves more than just these. Patients also experience non-motor symptoms, such as cognitive impairment, anxiety, depression, fatigue, and sleep problems.

Myth 3: PD only affects one part of the brain (the substantia nigra pars compacta).
Fact: PD primarily targets the substantia nigra pars compacta in the brain, leading to motor symptoms such as tremors and rigidity. However, the impact extends beyond, affecting various brain regions and causing a range of motor, cognitive, affective, autonomic, and sensory impairments.
Fact: Although PD lacks a cure, pharmacotherapy such as levodopa assist in symptom management. Contrary to a prevailing myth, levodopa can be effective for decades, but its potency may diminish due to disease progression, not a time limit. As PD advances, the enzyme converting levodopa to dopamine declines, affecting its efficacy over time. While the drug remains effective, the duration of symptom relief may shorten over time, leading to a phenomenon known as wearing-off, where symptoms return before the next dose.
Sources
Health Union Medical Editorial Team. Myths and Misconceptions About Parkinson’s. 2017. [Internet]. Available at: https://parkinsonsdisease.net/basics/ myths-misconceptions-facts
John’s Hopkins Medicine. Myths and Facts: 7 Parkinson’s Disease Misconceptions. 2024. [Internet]. Available at: https://www.hopkinsmedicine.org/health/ conditions-and-diseases/parkinsons-disease/myths-and-facts-7-parkinsondisease-misconceptions#:~:text=Myth%201%3A%20Parkinson’s%20is%20 %E2%80%9Conly,a%20lot%20more%20than%20that
Newman T. Medical Myths: All about Parkinson’s disease. 2021. [Internet]. Available at: https://www.medicalnewstoday.com/articles/ medical-myths-all-about-parkinsons-disease
Parkinson’s Foundation. Myths About Parkinson’s. 2024. [Internet]. Available at: https://www.parkinson.org/understanding-parkinsons/what-is-parkinsons/myths World Health Organization. Parkinson’s Disease. 2023. [Internet]. Available at: https://www.who.int/news-room/fact-sheets/detail/parkinson-disease
Fact: Despite persistent misconceptions suggesting that PD medications, particularly levodopa, accelerate the progression of the disease, extensive research has debunked this myth. Large clinical trials have demonstrated that individuals treated with levodopa do not experience a faster decline compared to those on a placebo. While not a cure, levodopa is a valuable therapy for managing motor symptoms without harmful effects.
Fact: While tremors are a characteristic of PD, not everyone diagnosed exhibits this symptom. Some individuals may never experience tremors, and even those who do may not manifest them initially.
Fact: A defeatist attitude that implies helplessness is counterproductive. Regular physical activity has been shown to significantly improve daily functioning for patients living with PD. Engaging in weekly exercise sessions can enhance overall well-being and quality of life.
Myth 8: PD is fatal.
Fact: While a diagnosis of PD is undoubtedly challenging, it is not a death sentence. PD itself is not directly fatal, but complications such as falls and infections can pose risks, particularly in later stages. Quality care, including exercise and regular check-ups, is crucial in managing the disease’s progression.
Myth 9: PD has spontaneous exacerbations, it can flare-up unexpectedly.
Fact: While PD may exhibit spontaneous exacerbations and unexpected flare-ups, the progression of PD is generally slow. Daily symptom fluctuations may occur, but if symptoms worsen over days or weeks, it is crucial to investigate potential underlying causes. Factors such as medication adjustments, infections, dehydration, sleep deprivation, recent surgery, stress, or other medical conditions can contribute to the exacerbation of PD symptoms. Notably, urinary tract infections, even in the absence of apparent bladder symptoms, are frequently identified as a common culprit.
Myth 10: Deep brain stimulation (DBS) is an experimental therapy.
Fact: DBS has been a well-established and successful procedure for decades. In DBS, electrodes are placed in the brain to address motor symptoms when medications become less effective. It operates similarly to a pacemaker but involves wires in the brain. DBS has been a standard therapeutic approach for over two decades.

Many of you will relate to this article. While we all may agree that vacation is a crucial rejuvenating activity, many of us end up working during our break from work. A new American study showed that the majority of physicians work during their annual vacations and end up burning out.
In theory, taking a vacation gives us an opportunity to detach from our daily grind, resulting in improved job performance, heightened productivity, increased creativity, enhanced job satisfaction, better personal relationships, reduced absenteeism, lower turnover rates, and arguably most importantly a decreased risk of burnout.
Additionally, taking vacations is linked to enhanced physical and mental health, resulting in a lower risk of cardiovascular
mortality, decreased cellular-level stress markers, and fewer symptoms of depression and anxiety.
Sinsky et al conducted a cross-sectional survey of American physicians between 2020 and 2021 to look at the link between the number of vacation days taken annually, the extent of work carried out during vacations, and their impact on physician burnout and professional fulfilment.
Of the 3024 respondents, 59.6% took ≤15 vacation days in a year, and 19.9% took
≤5 days. The majority (70.4%) engaged in patient care related tasks during vacations, with 33.1% working ≥30 minutes on a typical vacation day.
Adjusting for personal and professional factors, concerns about finding coverage for clinical responsibilities and financial worries were associated with a decreased likelihood of taking >3 weeks of vacation annually.
Taking more >3 weeks of vacation, having full inbox during vacation, and spending ≥30 minutes per vacation day on patient-related work were associated with lower rates of burnout. Conversely, extended time spent on patient-related work during vacations was linked to higher burnout rates.
The authors concluded that system-level efforts to ensure physicians take adequate vacation and have coverage for clinical responsibilities, including managing the inbox, may reduce physician burnout.

Irritable bowel syndrome (IBS) is a common chronic functional gastrointestinal disorder, now recognised as part of disorders of the gut-brain axis.
IBS has a multifactorial pathogenesis involving genetic, physiological, psychological, and environmental factors. The prevalence of IBS is higher in low- and middle-income countries, with variations in subtypes, such as IBSMixed and IBS-Constipation, and a higher prevalence in individuals of African descent.
Stress affects gut-brain interactions, leading to psychiatric comorbidities. Treatment recommendations include a personalised pharmacological approach to address individual symptoms and psychological interventions such as cognitive behavioural therapy and hypnotherapy.
Stress-management interventions and
pharmacological treatments targeting both gastrointestinal and psychological symptoms are essential.
Please note, this is just a summary of the article. To read the full article and answer the quiz go to https://www.medicalacademic.co.za/ courses/a-2-way-street-stress-and-ibs/ SF
When anxiety and stress creep in IBS symptoms flare up
1
IBS accounts for at least 20 % of outpatient gastroenterology clinic referrals 2
• In patients with IBS, the gut microbiome is associated with psychological distress, anxiety and depression 2
• IBS is caused by a disruption in the gut-brain axis (BGA) 3
• Neurotransmitters play an important role in regulating the microbiota-gut-brain axis 3
• Dysregulation of the gut microbiota plays a role in IBS 2
Relieving the spasm and stress of IBS is a simple 2-in-1 tablet taken 2-4 times daily Librax®, the 2-in-1 treatment for stress-related IBS, combines the anti-anxiety action of chlordiazepoxide and the antispasmodic effects of clinium bromide.
*IBS - Irritable Bowel Syndrome

References: 1. Arishi AM, Elmakki EE, Hakami OM, Alganmy OM, Maashi SM, Al-Khairat HK, et al. Irritable Bowel Syndrome: Prevalence and Risk Factors in Jazan Region, Saudi Arabia. Cureus. 2021;13(6):e15979. 2. Shaikh SD, Sun N, Canakis A, Park WY, Weber
S5 Librax® (Tablets), B994 (Act 101/ 1965). Each tablet contains 5 mg chlordiazepoxide & 2,5 mg of clidinium bromide. For full prescribing information refer to the Professional Information approved by the Medicines Regulatory Authority. Viatris South Africa (Pty) Ltd. Reg. No.: 1991/003162/07.
Irritable bowel syndrome (IBS) is considered a complex condition involving both peripheral and central factors. The gut-brain axis (GBA), a two-way neurohumoral communication system that links the functions of the brain and gastrointestinal (GI) tract, impacts gut motility, appetite, and weight. The gut microbiota mediate communication between the gut and brain.1,2
The bidirectional communication network of the GBA comprises the central nervous system (CNS), the autonomic nervous system (ANS), the enteric nervous system (ENS) – often referred to as the ‘second brain’ due to its extensive network of neurons in the GI tract –and the hypothalamic-pituitary-adrenal axis.2,3
Typically, communication from the gut to the CNS occurs autonomously and goes unnoticed by the individual. However, in pathological conditions such as IBS, signals may extend to the somatic sensory system, resulting in symptoms like discomfort, nausea, and pain. Conversely, the CNS output through the ANS can contribute to GI dysfunction.2
Microbial molecules transmit signals to the brain via vagal and afferent nerve pathways, as well as through cytokines and neurotransmitters. Gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the CNS, is found not only in the brain but also in the GI track. It reduces neuronal excitability and has been linked to various physiological functions in the GI tract including IBS. 2,3,4
GABA serves diverse functions in the GI track, including modulating visceral nociception, colonic afferent excitability, GI secretion, motility, and supporting the local immune system.5
GABA transporters (GAT) in the gut, such as GAT2 in enteric glia cells and GAT3 in myenteric neurons, regulate GABAergic signalling. Altered GABA levels are associated with inflammatory diseases, including decreased levels in multiple sclerosis, ischaemic stroke, and ulcerative colitis.5
In patients with IBS, particularly IBSDiarrhoea subtype, GABA, glutamic acid decarboxylase 2, GABA-B receptors, and GAT-2 are dysregulated, suggesting a
link between stress-induced GABAergic alterations and IBS pathogenesis.5
Chronic pelvic pain patients with lower GABA levels in the anterior cingulate cortex highlight the association between GABA and visceral pain hypersensitivity, a key symptom in IBS.5
Anxiety disorders or stress, commonly comorbid with IBS, show increased GABA levels in the prefrontal cortex in severe cases, indicating a potential link between GABAergic alterations and anxiety-related IBS manifestations.5
While GABA is a significant player, the GBA involves a complex interplay of various neurotransmitters. Other key neurotransmitters associated with IBS include:3,5
_ Serotonin (5-HT): Abnormalities in serotonin signalling have long been implicated in IBS. Serotonin regulates bowel movements, and alterations in its levels or receptor sensitivity may contribute to IBS symptoms.
_ Dopamine: Dopaminergic pathways are also involved in gut motility and sensation. Imbalances in dopamine levels may impact the GBA and contribute to IBS symptoms.
_ Glutamate: As the primary excitatory neurotransmitter in the CNS, glutamate plays a role in pain perception. Changes in glutamatergic signalling may contribute to visceral hypersensitivity seen in IBS.
_ Acetylcholine: Involved in smooth muscle contraction, acetylcholine abnormalities may influence gut motility. Dysregulation in cholinergic signalling is associated with IBS.
_ Histamine: Histamine receptors are present in the gut and are involved in immune responses. Histamine dysregulation may contribute to GI symptoms in IBS.
_ Norepinephrine: In the peripheral nervous system, noradrenergic neurons respond to stress, impacting various physiological functions. In the gut, norephinephrine affects digestive function through β3receptors, leading to reduced motility.
However, acute stress stimulates colonic contractile activity, influencing defecation. Dysregulation of norephinephrine in IBS involves α2A-adrenoceptor alterations, impacting colonic norephinephrine release.
Understanding the role of neurotransmitters, including GABA, in IBS opens avenues for potential therapeutic interventions. Targeting neurotransmitter systems could offer novel approaches to manage symptoms and improve the quality of life for individuals with IBS.
Pharmacotherapy modulating GABAergic neurotransmission or targeting other neurotransmitter systems may be explored. However, developing drugs that specifically target the gut without affecting the central nervous system poses a challenge.
Probiotics, which influence the gut microbiota, have shown promise in managing IBS symptoms. The gut microbiota can impact neurotransmitter production and signalling, providing a potential avenue for intervention.
Certain dietary components, such as fermented foods and prebiotics, may positively influence GABAergic neurotransmission. Dietary strategies focusing on neurotransmitter modulation could complement existing treatments.4
The GBA and the role of neurotransmitters, including GABA, in the pathophysiology of IBS highlight the intricate connection between the gut and the CNS.
References available on request. SF
The global prevalence of major depressive disorder, anxiety disorders and IBS is increasing1
Since 2021, there has been a 35 % increase in the number of South Africans who feel distressed or are ‘struggling‘ 2 In 2022, ranked as one of the lowest of 64 countries in terms of mental well-being** 2
Leading causes of stress among South African Professionals were: The high cost of living, followed by unreliable electricity supply*** 3

1
Those with depression:^
Are twice as likely to develop new-onset IBS
Have a two-fold higher risk of comorbid IBS
References: 1.
S5 Librax® (Tablets), B994 (Act 101/1965). Each tablet contains 5 mg chlordiazepoxide & 2,5 mg of clidinium bromide.
full prescribing information refer to the Professional Information approved by the Medicines Regulatory Authority.

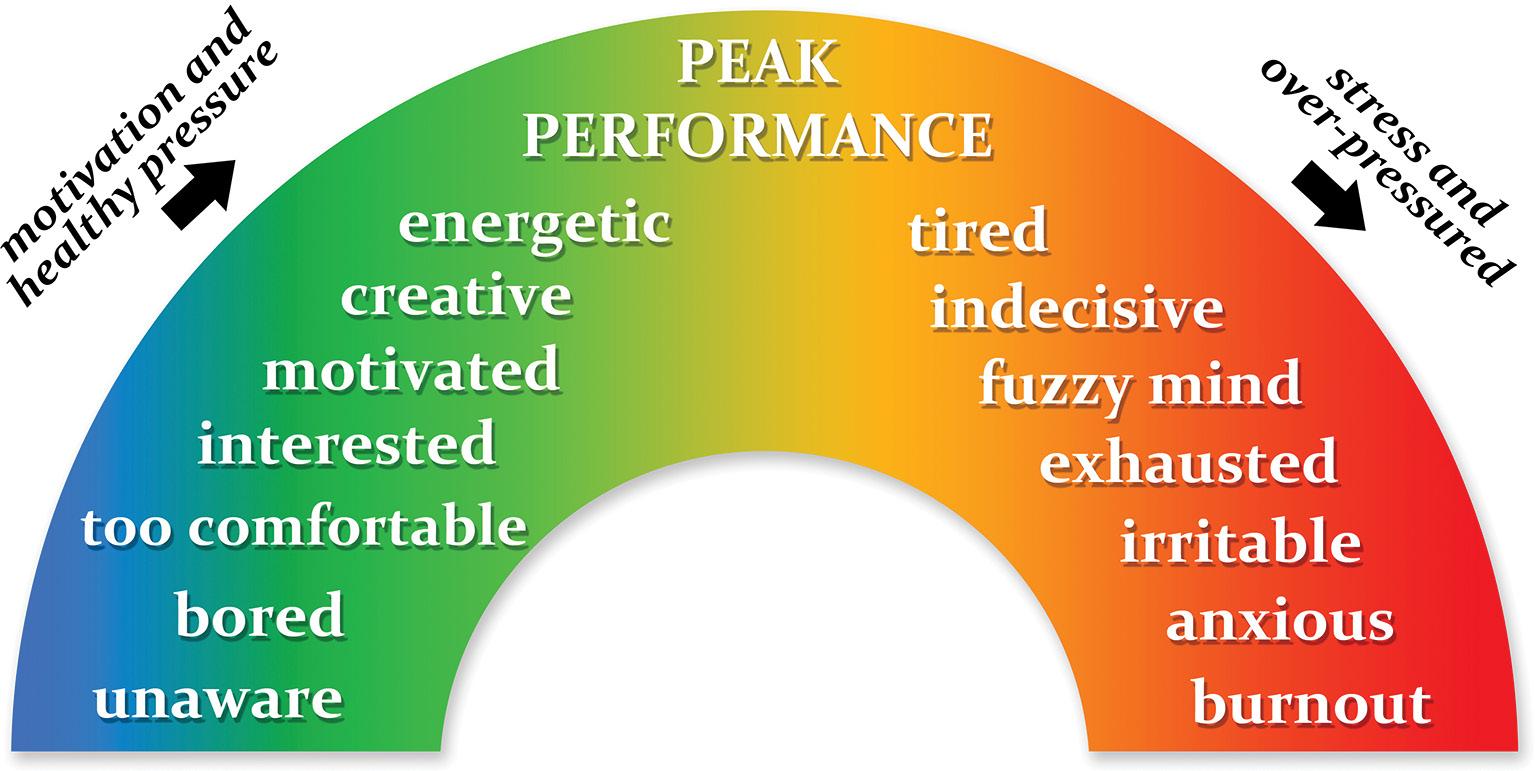
The global prevalence of acne is estimated to be as high as 95% –depending on the population studied and the definition of acne used. Acne typically manifests at the onset of puberty. While it commonly resolves after this period it can persist in adulthood (~40% of adults aged between 30- and 39-years still experience its effects).1
A recent survey found that the severity of acne, and its occurrence in individuals with darker skin tones, are associated with high levels of stigmatisation. According to Shields et al, respondents perceived individuals with severe acne as having poor hygiene, being unattractive, unintelligent, unlikable, immature, and untrustworthy. Furthermore, respondents indicated that they were more inclined to socially distance themselves from dark skinned individuals living with acne. 2
The team concluded that strategies to diminish stigmatising attitudes, and ensuring sufficient access to care, are crucial for the effective management of acne and its psychological sequelae. 2
Another survey – this time among individuals living with acne – found that only ~30% of participants have ever consulted a dermatologist about their disease, indicating a potential gap in accessing effective treatments. 3
Notably, 60% felt they had to ‘just deal with’ acne, and 54% believed it was not preventable. While 85% recognised
According to the Global Burden of Disease study, acne, an inflammatory condition affecting the pilosebaceous unit, is associated with a significant psychological burden - especially in younger individuals. Despite being a common dermatological disease, stigmatisation of individuals living with acne unfortunately persist.1,2
hormones as a cause, 69% attributed acne to sweat, 30% believed eliminating junk food could cure it and 35% believed squeezing pimples would help. 3
Survey results also indicated that many participants used unreliable sources to search for information about their disease. Around 45% relied on search engines, 43% sought advice from friends and family, and 20% were influenced by social media –particularly TikTok and Instagram. 3
Among those following a skincare routines, <20% considered themselves ‘very successful’ in preventing acne. Acne-related self-consciousness led to social avoidance for 30%, with 55% feeling self-conscious on video calls, 48% hiding from cameras, and 38% using filters to conceal acne in photos. 3
Primary care physicians play a crucial role in managing acne, especially in identifying cases that require specialised attention. History-taking plays a crucial role in assessing and treating acne, as well as identifying potential triggers. 5
Obtaining detailed information about aggravating and causative factors is essential to rule out systemic disorders and medication-induced acne. Women should be asked about symptoms of hyperandrogenism, and variations in acne severity should be assessed, especially during hormonal swings in pregnancy and menopause.4,5
Occupational history can reveal exposure to substances causing acne, such as oils and greases (chloracne) or friction and
pressure on the skin (acne mechanica). Furthermore, a thorough history of previous treatments is vital, as patients often selftreat with over-the-counter medications. 5
Understanding treatment failure or relapse involves exploring the medications used, their type (topical versus systemic), dosage, frequency, duration, compliance, and adverse effects experienced. 5
Psychosocial assessment is also crucial. Clues to potential issues include poor eye contact, limited speech, anger, poor personal hygiene, and verbal self-deprecation. Explicit questioning about low mood and anhedonia
Table 1: Acne Severity Scale 6
Grade Description
Grade 1 Also known as comedones, and is categorised into two types, open and closed. Open comedones form when the pilosebaceous orifice becomes plugged with sebum and appears as papules with a central, dilated follicular orifice containing grey, brown, or black keratotic material. On the other hand, closed comedones form when keratin and sebum block the pilosebaceous orifice beneath the skin surface. They appear as dome-shaped, smooth papules that can be skin-coloured, whitish, or greyish in appearance
Grade 2 Inflammatory lesions present as a small papule with erythema
Grade 3 Pustules
Grade 4 Many pustules coalesce to form nodules and cysts called nodulocystic acne

is necessary, and tools are available to assess psychosocial function effectively.5
Clinical features to look out for include polymorphic lesions like comedones, papules, pustules, nodules, and pseudocysts, often developing from sebaceous glands associated with hair follicles. Severity can be assessed using an acne severity scale (see Table 1). 5,6
Treatment goals involve actively managing acne to reduce lesions, improve psychosocial symptoms, and prevent scarring. As mentioned, acne has a profound psychological impact on individuals – especially young people. Evidence suggests that appropriate acne treatment can alleviate these negative psychological consequences.4,5
Treatment options depend on factors like age, gender, disease severity, duration, and tolerability, with various agents and formulations available. Addressing myths (see Table 2) associated with acne management is crucial during treatment. 5
The American Academy of Dermatology (AAD) and the National Institute for Health and Care Excellence (NICE) recently updated their treatment guidelines (see Tables 3 and 4).7,8
Topical therapies Topical retinoids, benzoyl peroxide (BP), antibiotics, clascoterone, salicylic acid, and azelaic acid are the mainstays of acne treatment. Multimodal therapy combining multiple mechanisms is recommended. Topical retinoids are effective but may cause side effects. BP is antimicrobial and comedolytic. Topical antibiotics are recommended but not as monotherapy due to the risk of resistance. Fixed-dose combinations are useful
Topical retinoids Comedolytic, anti-inflammatory, and improve dyspigmentation. Types include tretinoin, adapalene, tazarotene, and trifarotene. Used as monotherapy or in combination. Side effects include dryness, erythema, and peeling. No superiority of one retinoid over another
Benzoyl peroxide (BP)
Washing the face will reduce acne
Antibiotic cream is the best treatment
Long-lasting cosmetics and sunscreens are recommended for individuals living with acne
Squeezing or popping ‘ripe’ pimples will speed healing
Redness experienced after topical acne treatment is a sign of an allergy
One to two pimples is/are not a big deal
Excessive cleaning increases dryness and may increase colonisation of Cutibacterium acnes
Topical antibiotics will increase resistance to antibiotics, thereby affecting the efficacy of treatment. Antiseptics are preferred
Occlusive applications should be avoided as they may encourage comedone formation
Squeezing can result in cystic lesions and scarring
Skin irritations and solar sensitivity are known side effects of many topicals. Temporary cessation or lengthening of the frequency of application may be necessary after a review assessment
To the affected individual it does. A supportive consultation and useful advice may make a lot of difference
Releases free oxygen radicals and is mildly comedolytic. Used for inflammatory and noninflammatory lesions. Side effects include burning sensation and dryness. Concentration and formulation impact tolerability
Topical antibiotics Include erythromycin, clindamycin, minocycline, and dapsone. Treat acne through antibacterial and anti-inflammatory effects. Used in combination with BP to prevent resistance. Side effects are generally low. Monotherapy is not recommended due to the risk of resistance
Fixed-dose topical combinations Combinations of BP, retinoids, or antibiotics for adherence. Examples: BP and topical retinoid, BP and topical antibiotic, topical retinoid and topical antibiotic. Combined therapy enhances efficacy. Use of BP with combinations is recommended to prevent resistance
Clascoterone Inhibits lipid and inflammatory cytokine synthesis. Cost may impact access
Salicylic acid Used in concentrations of 0.5% to 2%. Improves inflammatory lesions and comedones
Azelaic acid Helpful for sensitive or darker skin types. Lightening effect on dyspigmentation
Systemic antibiotics Used for moderate to severe acne. Tetracycline-class antibiotics like doxycycline, minocycline, and sarecycline. Antibiotic and anti-inflammatory effects. Concerns about antibiotic resistance and complications. Limit use and consider concomitant topical therapies
Doxycycline Gastrointestinal disturbances are common side effects and phototoxicity. Consideration of dosage variations is needed
Minocycline Conditionally recommended due to moderate certainty of benefits but concerns about rare adverse effects. Rare adverse effects include vertigo, autoimmune hepatitis, and skin hyperpigmentation
Sarecycline Conditionally recommended due to high certainty of benefits. Well-tolerated with low incidence of side effects. Cost may impact access
Furthermore, NICE recommends considering topical BP monotherapy as an alternative for severe acne if contraindicated or the individual prefers to avoid retinoids or antibiotics. For moderate-to-severe acne consider trimethoprim or an oral macrolide as replacements in combination treatments if oral lymecycline or doxycycline are contraindicated.8
Combined oral contraceptives (COCs) COCs consist of oestrogen and progestin and act by inhibiting gonadotropin-releasing hormone, follicle-stimulating hormone, and luteinizing hormone to prevent ovulation and pregnancy. Their anti-androgenic properties are key in treating acne, reducing ovarian androgen production, increasing sex hormone-binding globulin, and lowering free testosterone that activates the androgen receptor. COCs also diminish 5α -reductase activity and block the androgen receptor.7
Oethinyl oestradiol, the oestrogen component in COCs, is typically dosed from 10-50μg daily. Progestins are synthesised progesterone analogues. COCs with first, second, and third-generation progestins are derived from testosterone, potentially having androgenic effects if used alone. Notably, fourth-generation progestins like drospirenone exhibit antiandrogenic properties, according to the AAD. Studies show that COCs significantly reduced inflammatory/non-inflammatory lesion counts compared to placebo.7
Spironolactone
Spironolactone, an aldosterone receptor antagonist, acts by decreasing testosterone production and inhibiting its binding to androgen receptors. Studies show improvement in acne severity compared to placebo. Common side effects include menstrual irregularities, breast tenderness, and diuresis. Notably, spironolactone should be avoided during


Severity Treatment
Any severity Topical adapalene with topical BP (once daily, evening)
Any severity Topical tretinoin with topical clindamycin (once daily, evening)
Mild to moderate Topical BP with topical clindamycin (once daily, evening)
Moderate to severe Topical adapalene with topical BP (once daily, evening) + oral lymecycline or doxycycline (once daily)
Moderate to severe Topical azelaic acid (twice daily) + oral lymecycline or doxycycline (once daily)
Advantages
ñ Topical application
ñ No antibiotics
Topical application
ñ Topical application
ñ Caution during pregnancy and breastfeeding
ñ Oral component for hard-to-reach areas
ñ Systemic antibiotics
ñ Oral component for hard-to-reach areas
ñ Systemic antibiotics
pregnancy, and concurrent use with COCs is often recommended. Potassium monitoring should be considered in specific patient groups, including older individuals or those with medical comorbidities.7
Isotretinoin is approved for the treatment of severe nodular acne. Its mechanisms include sebaceous gland size reduction, decreased sebum production, and antiinflammatory properties. Isotretinoin is considered highly effective, especially for severe or scarring acne.7
Use affects the mucocutaneous, musculoskeletal, and ophthalmic systems. Laboratory monitoring, including liver function tests and fasting lipid panels, is recommended during treatment. Use is not recommended during pregancy.7
The AAD guidelines reviewed various interventions, including acne lesion extraction, chemical peels, laser and lightbased devices, microneedle radiofrequency devices, and photodynamic therapy with aminolaevulinic acid. According to the authors, the available evidence was deemed insufficient to formulate recommendations for or against these modalities.7
In terms of complementary and alternative therapies, including botanical agents and vitamins, for acne treatment, the authors state that once again, insufficient evidence precluded the
Disadvantages
ñ Not suitable during pregnancy
ñ Caution during breastfeeding
ñ Skin irritation, photosensitivity, bleaching
ñ Not suitable during pregnancy or breastfeeding
ñ Skin irritation, photosensitivity
Skin irritation, photosensitivity, bleaching
ñ Not for use in pregnancy, breastfeeding, or <12-year
ñ Skin irritation, photosensitivity, bleaching
ñ Systemic side effects, antibiotic resistance
ñ Not for use in pregnancy, breastfeeding, or <12-years
ñ Systemic side effects, antibiotic resistance
development of specific recommendations regarding the use of topical tea tree oil, topical green tea, topical witch hazel, oral pantothenic acid, oral or topical zinc, and oral or topical niacinamide.7
While some studies showed improvements in acne scores and lesion counts with a low-glycaemic-load diet, others found no significant differences. The evidence base for other dietary interventions, such as low dairy diet, low whey diet, omega-3 fatty acids, and chocolate, was also deemed insufficient to draw conclusive recommendations for acne treatment.7
Acne not only poses a physical but also a significant psychological burden, particularly impacting individuals during adolescence and adulthood. Stigmatisation persists, influencing social and professional interactions. Studies reveal that severe acne is associated with negative perceptions, affecting individuals’ self-esteem, attractiveness, and likability. The importance of addressing and reducing stigmatising attitudes is emphasized to improve the wellbeing of those living with acne.
Access to care remains a concern, with a considerable percentage of individuals not consulting dermatologists. Misconceptions about acne, including its preventability and causes, contribute to suboptimal careseeking behaviour. The impact of social media and misinformation sources on acne-related perceptions and treatments is notable.
Primary care physicians play a vital role in managing acne, with thorough
history-taking, psychosocial assessment, and clinical evaluation essential for effective treatment.
A number of effective treatments are available. The choice of treatment depends on individual factors. Physical modalities, complementary therapies, and dietary interventions lack sufficient evidence for clear recommendations, highlighting the need for further research in these areas. Overall, appropriate acne treatment is crucial not only for reducing lesions but also for addressing the profound psychological impact, improving psychosocial symptoms, and preventing scarring.
1. Witkam WCAM, Dal Belo SE, Pourhamidi S, et al. The epidemiology of acne vulgaris in a multiethnic adolescent population from Rotterdam, the Netherlands: A cross sectional study. J Am Acad Dermatol, 2024.
2. Shields A, Nock MR, Ly SL, et al. Evaluation of Stigma Toward Individuals With Acne. JAMA Dermatol, 2024.
3. Sun Pharma Press Release. Sun Pharma Survey Reveals Americans with Mild-to-Moderate Acne Have Defeatist Attitudes About Treatment, Despite Self-Consciousness. 2023. [Internet]. Available at: https://www.prnewswire.com/news-releases/sunpharma-survey-reveals-americans-with-mild-tomoderate-acne-have-defeatist-attitudes-abouttreatment-despite-self-consciousness-301975000. html#:~:text=PRINCETON%2C%20N.J.%2C%20 Nov.%202,acne%2C%20despite%20feelings%20 of%20self%2D
4. Moosa AS, Lim SF Koh YLE, et al. The management of acne vulgaris in young people in primary care: A retrospective cohort study. Front Med, 2023.
5. Moosa AS, Quah JHM, How CH. Primary care approach to managing acne. Singapore Med J, 2021.
6. Sutaria AH, Masood S, Saleh HM, et al. Acne Vulgaris. Updated 2023 Aug 17 [Internet]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK459173/
7. Reynolds RV, Yeung H, Cheng CE. Guidelines of care for the management of acne vulgaris. JAAD, 2024.
8. NICE. Acne vulgaris: management guidelines. Updated 2023. [Internet]. Available at:
https://www.nice.org.uk/guidance/ng198/ chapter/Recommendations SF
Scan for the quiz



Among the malignancies linked to rosacea, a 2023 review by Thapa et al reports an increased risk of basal cell carcinoma (41%), squamous cell carcinoma (33%), breast cancer (8%), and melanoma (8%). Furthermore, rosacea has been associated with a higher likelihood of comorbidities, including cardiovascular, gastrointestinal, neurologic, psychiatric, and autoimmune diseases. Psychiatric comorbidities such as depression, social phobia, and anxiety significantly impact the quality of life for affected individuals.
Rosacea presents with various phenotypes, including erythematotelangiectatic, papulopustular, phymatous, and ocular. Each phenotype involves distinct manifestations, such as flushing, persistent facial erythema, papules, pustules, thickened skin with enlarged pores, and ocular symptoms like watery or bloodshot eyes. Ocular rosacea can occur with or without other forms of rosacea and may involve symptoms such as foreign body sensation, burning, and stinging.
Rosacea, a chronic skin condition primarily affecting individuals with Fitzpatrick skin types I and II and those with photosensitive skin, has been associated with a heightened risk of malignancies and comorbidities, according to a recent study. The prevalence of rosacea is ~5.46% in the general population and is more common in
The pathogenesis of rosacea is complex and involves factors like skin barrier dysfunction, environmental/genetic triggers, and the interplay of antimicrobial peptides, particularly cathelicidins. The peptide LL-37, derived from cathelicidins, plays a crucial role in initiating and activating rosacea by inducing inflammation, angiogenic chemokine release, and mast cell activation. Transient receptor potential (TRP) channels, especially TRPV4, and mast cell activation and degranulation also contribute to the pathogenesis.
Various triggers can exacerbate rosacea, including dietary factors like hot drinks, alcohol, spicy foods, and certain chemicals. Sun exposure, an intestine-skin connection, and external factors like face masks can worsen symptoms.
Managing rosacea is challenging and involves a multifaceted approach. This includes general skincare education, sun protection, moisturizers, and trigger avoidance. Treatment modalities range from systemic and topical therapies to laser
and light-based treatments, depending on the specific phenotypic features.
Understanding the association between rosacea and malignancies/comorbidities, recognising its diverse phenotypes, elucidating its complex pathogenesis, and addressing triggers are crucial in managing this chronic skin condition. The multi-faceted approach recommended by the global Rosacea Consensus panel aims to improve the quality of life for individuals living with rosacea by addressing both cutaneous and associated systemic manifestations.
Please note, this is just a summary of the article. To read the full article, go to www. medicalacademic.co.za. SF

Contact urticaria (CU) is a transient wheal and flare reaction that occurs within 10 to 60 minutes at the site of contact of the triggering agent and completely resolves within 24 hours. CU is a form of acute urticaria (symptoms last for >6 weeks).1
The prevalence of occupational CU is 0.4% and accounts for 30% of all occupational skin diseases. Healthcare professionals as well as those involved in lab work, agriculture, hairdressing, the cosmetic, chemical cleaning, construction, catering, cooking, electronics, machinery, and metal products industries are at highest risk of CU.1 Research indicates a prevalence of 5% to 10% for latex-related CU. The prevalence of sensitisation to natural rubber latex (NRL) among healthcare workers is between 5% to 13%. NRL, cosmetics, skin creams, and sorbic acid are some of the most common causative agents identified.1
Based on pathophysiology, UC are categorised into:1
1 Immunologic CU (ICU): Involves antigen binding to immunoglobulin E (IgE)-specific antibodies on mast cells, leading to histamine release and skin microcirculation disturbance. It progresses through stages, from localised urticaria to generalised anaphylactic reactions. High molecular weight proteins (eg dietary proteins) and hapten chemicals (eg diisocyanate) are common triggers.
2 Non-immunologic CU (NICU): Less severe and more common, with no specific antibodies against causative agents. Non-steroidal anti-inflammatory drugs inhibit the response, suggesting a role for prostaglandins in pathogenesis. Unlike ICU, NICU lacks systemic manifestations and remains localised. Agents include animals, foods, fragrances, medications, metals, plants, preservatives, and disinfectants.
3 CU due to unknown mechanisms: May involve IgE or classical pathway mediation. Overlapping causative agents exist between ICU and NICU.
The typical clinical presentation includes an itchy, often painful wheal and flare response, accompanied by angioedema. Patients may manifest hives (urticaria) or dermatitis (eczema).1 A wheal has three typical features:2
_ A sharply circumscribed superficial central swelling of variable size and shape, almost invariably surrounded by reflex erythema
_ An itching or sometimes burning sensation
_ A fleeting nature, with the skin returning to its normal appearance, usually within 30 min to 24 hours.
Angioedema is characterised by:2
_ A sudden, pronounced erythematous or skin-coloured deep swelling in the lower dermis and subcutis or mucous membranes
_ Tingling, burning, tightness, and sometimes pain rather than itch
_ A resolution slower than that of wheals (can take up to 72 hours).
Step 1
The diagnostic process for urticaria begins with a comprehensive history. Using questionnaires can be beneficial in obtaining detailed information. 2
Step 2 Involves a thorough physical examination. Given the transient nature of wheals and angioedema, which may not be present during the examination, it is crucial to review any documented signs and symptoms, including photographic evidence of wheals and/or angioedema. Skin examination should consider the site of involvement, lesion distribution, size, shape, confluency, angioedema, erythema, pallor, dermographism, and urticarial vasculitis.1,2
Step 3 A basic diagnostic workup incorporating limited tests is recommended, which include differential blood count, erythrocyte sedimentation rate and/or C-reactive protein, immunoglobulin G antibodies against thyroid peroxidase, and total IgE. Further diagnostic tests, tailored to individual cases, may be considered based on the findings from the initial three steps.
CU management involves a multi-faceted approach with a focus on prevention and pharmacological interventions. Key principles include identifying the causative agent, eliminating exposure through avoidance or preventive measures, and controlling symptoms through conservative or pharmacologic means. Upon identification of


the culprit, patients must be educated about their condition’s potential evolution and available therapeutic options.3
For ICU, recurrent exposures can escalate to subsequent stages, increasing the risk of anaphylaxis. Patients with ICU should be advised to carry injectable epinephrine and antihistamines (AHs) for potential lifethreatening reactions.3
Primary prevention centres around complete avoidance of the triggering agent, although this may be challenging in occupational settings. Protective skin measures like gloves or pharmacologic prophylaxis are recommended.3
Pharmacologic treatments for CU –particularly ICU – focus on inhibiting inflammatory mediator release. First-line medications include second-generation H1 AHs, which effectively block histamine’s local and systemic effects. Dose optimisation is crucial, and severe cases may require short courses of oral steroids.
NICU can be managed with aspirin and non-steroidal anti-inflammatory drugs to counteract prostaglandin and leukotriene inflammatory effects.3
Alternative therapies like ultraviolet light, leukotriene receptor antagonists, and immunomodulators have not been extensively studied for CU. Subcutaneous immunotherapies for specific urticants, such as occupational flour allergy and latex-induced CU, are undergoing evaluation, showing promise in some studies. However, standard recommendations and consensus on the efficacy of these alternative therapies in CU are currently lacking.3
CU has a significant impact on individuals, particularly those in high-risk occupational sectors. Beyond its physical manifestations, CU affects patients’ quality of life. The diagnostic process involves a comprehensive history, thorough physical examination, and a tailored diagnostic workup. Effective management includes primary prevention through avoidance and secondary prevention with pharmacological interventions. AHs remain the cornerstone of controlling symptoms.
References available on request. SF

An estimated one billion people worldwide are living with obesity – 650 million adults, 340 million adolescents and 39 million children. By 2025, an estimated 167 million people will be directly affected by being overweight or living with obesity.1 as type 2 diabetes (T2DM), hypertension, cardiovascular disease (CVD), osteoarthritis, pulmonary diseases and cancer.2,3,4
Individuals with a BMI ≥25kg/m2 have an increased risk of early mortality. South
African data show that 57.4% of deaths were attributed to NCDs in 2016, of which ~60% occurred in individuals <70-years.4
An analysis showed that 87% of South Africans died as a result of obesityassociated T2DM, 68% of hypertension, 61% of endometrial cancer, 45% of ischaemic stroke, 38% of ischaemic heart disease, 31% of kidney cancer, 24% of osteoarthritis, 17% of colorectal cancer, and 13% of post-menopausal breast cancer.4
Individuals living with obesity also face physical limitations and the risk of psychiatric disorders associated with stigmatisation and social discrimination. Psychiatric disorders such as anxiety, eating disorders, and depression frequently cooccur in individuals living with obesity. Research consistently shows substantial rates of co-occurrence, ranging from 20% to 60% for bipolar mood disorder, 30% to 70% for psychotic disorders, and 20% to 50% for depression.4,5
Childhood and adolescent obesity pose a risk for various health complications, including early puberty, menstrual irregularities, and polycystic ovary syndrome in female adolescents.5
Additionally, obesity is associated with conditions such as obstructive sleep
apnoea and metabolic syndrome. More than 80% of adolescents living with obesity are likely to continue experiencing these health concerns into adulthood. 5
Guideline recommendations
International guidelines recommend the use of anti-obesity medications (AOM) for individuals with a BMI ≥30kg/m². AOM may also be considered for those with a BMI of >27kg/m² or higher if accompanied by one or more comorbid medical conditions.6
Approved AOMs in South Africa include orlistat, phentermine, combination naltrexone and bupropion, as well as liraglutide. Orlistat primarily exerts its effects peripherally by inhibiting gastric and pancreatic lipases, resulting in reduced absorption of dietary fat.6
According to Nguyen et al, the precise mechanism through which phentermine mitigates obesity remains unclear. Phentermine acts as an indirect sympathomimetic agent, enhancing the release of norepinephrine from presynaptic vesicles in the lateral hypothalamus and impeding its reuptake.7
The increase in norepinephrine concentration within the synaptic cleft activates β -2 adrenergic receptors, leading to appetite inhibition. While some reports suggest that phentermine may inhibit neuropeptide Y, a key player in hunger induction, the precise mechanism remains unclear.7
Additionally, phentermine induces the release of serotonin and dopamine from nerve terminals and serves as a weak, reversible inhibitor of monoamine oxidase and serotonin reuptake.7
Phentermine is well-absorbed through the gastrointestinal tract, with 80% excreted unchanged in urine. It has a half-life of 20 hours and is distributed to all tissues, including the brain.7
The combination of naltrexone/ bupropion enhances pro-opiomelanocortin peptide production, reducing food intake. This combination also influences reward



pathways, as well as self-control and awareness of fullness signals. 6
Glucagon-like peptide receptor (liraglutide) act centrally to reduce appetite and peripherally to enhance insulin secretion and decrease intestinal motility, leading to delayed gastric emptying. 6
In South Africa, phentermine is recommended as a short-term adjunct to a medically supervised comprehensive weight reduction programme, which should include exercise, diet (caloric/kilojoule restriction), and behaviour modification. 8
The recommendation is particularly applicable to individuals living with obesity (BMI ≥30kg/m2), who to do not have a satisfactory clinical response with a suitable weight reduction programme on its own. In cases where there are additional risk factors, consideration may be given to initiating phentermine treatment at a lower BMI. Phentermine is not recommended for children <12-years. 8
Numerous studies have investigated the efficacy of phentermine for weight reduction. A study by Weintraub et al (1984), explored the treatment of obesity with a combination of low dose phentermine and fenfluramine. The study compared different regimens: Phentermine resin (30mg in the morning), fenfluramine hydrochloride (20mg three times a day), a combination of phentermine resin (15mg in the morning) and fenfluramine hydrochloride (30mg before the evening meal), and a placebo.9
Phentermine monotherapy (10.0 +/- 1.2kg) and fenfluramine (7.5 +/- 1.2kg) resulted in greater weight loss compared to placebo (4.4 +/- 0.9 kg). Combination therapy resulted in greater weight loss.9
In their study, Kim et al (2006) assessed the effects of phentermine on weight reduction and safety in healthy patients living with obesity (BMI ≥25kg/ m²). Participants were randomised to phentermine 37.5mg or placebo once daily, along with behavioural therapy.10
The phentermine-treated group showed significant reductions in weight reduction (7kg) and waist circumference (3.5cm) compared to the placebo group (2-3kg). A notable percentage of participants in the phentermine group achieved a weight reduction of >5% compared to the placebo (85.7 vs 16%) and >10% (50% vs 8.3%) from baseline.10
Kang et al (2010) conducted a randomised, double-blind, placebocontrolled trial to evaluate the efficacy and safety of phentermine diffuse-controlled release (DCR), in patients living with obesity.
Results showed significant reductions in body weight (8.1kg) and waist circumference (0.5cm) in the DCR phentermine group compared to the placebo group.11
Additionally, the DCR phentermine group exhibited improvements in lipid profiles. The study concluded that short-term phentermine DCR treatment resulted in substantial weight reduction and metabolic improvement without severe adverse events.11
In a post-marketing surveillance study, Kim et al (2013) investigated the efficacy of phentermine in patients with living with obesity. A total of 45.6% of participants achieved a weight loss of ≥5%. The mean weight loss was 4kg.12
In a retrospective chart review, Ryder et al (2017) assessed the efficacy of phentermine as an adjunct to standard-of-care lifestyle modification therapy in adolescents with obesity. Results showed that phentermine use was associated with a significant decrease in BMI at month 1 (-1.6%), month 3 (-2.9%), and month 6 (-4.1%) compared to standard-ofcare lifestyle modification therapy alone.13
One of the main concerns about the use of AOMs include potential CV events. In response to these concerns, both the American Food and Drug Administration and the European Medicines Agency have revised their regulatory approval criteria for AOMs. These revisions emphasise the critical importance of ensuring CV and central nervous system safety in the evaluation and approval of these medications.6
Subsequent studies did not find any adverse CV outcomes, and phentermine continues to be one of the most frequently prescribed long-term AOMs.14,15
Hendricks et al (2011) assessed whether phentermine increases BP and heart ratepotentially increasing the risk of CVD. They collected data patients prescribed a lowcarbohydrate ketogenic diet or phentermine and analysed BP, heart rate, and weight changes during the first 12 weeks of therapy.16
Results indicated that participants in the phentermine group actually experienced a decline in systolic and diastolic BP. Heart rate changes were not significant. Weight reduction was significantly greater in the phentermine-group throughout the 104 weeks of the study.16
More recently, Lewis et al (2019) compared short- and long-term phentermine use, weight reduction, and the risk of CVD or CV-associated death. The primary outcome was per cent change in weight from baseline, measured at months 6, 12, and 24 after initial phentermine dispensing. Baseline BMI was 37.8kg/m2, 21% had a diagnosis of
hypertension at baseline, and 12% had a diagnosis of diabetes.17
Analysing electronic health records of adult patients (n=13 972) treated with phentermine, the team categorised users based on duration with ≤3 months as the reference group. By month six after initiation (or ~3 months after discontinuing phentermine), short-term users averaged 2.7% total weight loss.17
By month 12, their weight loss was 1.4% and no difference was noted at month 24. At month six, short-term intermittent users lost 1.8% additional body weight relative to short-term single episode (referent) users, while medium-term continuous users lost 5.1% more. At month 12, the mediumterm intermittent group lost 5.6% more weight than short-term single episode users. At month 12 long-term continuous (>12 months) users lost 7.4% more weight than short-term single episode users.17
By month 24, systolic BP in longer-term phentermine use groups for hypertensive patients was lower than among shortterm hypertensive users. Importantly, the occurrence of composite CVD or death was rare (0.3%), and there was no significant difference in risk between duration groups.17
Ritchey et al conducted a retrospective cohort study to assess the risk of major adverse CV events (MACE) associated with the use of combination phentermine and topiramate for weight management.18
Analysing insurance billing data, the study included patients aged >18-years with ≥6 months of continuous enrollment. The MACE rates among current users of phentermine and topiramate, fixed-dose phentermine/ topiramate, phentermine monotherapy, and topiramate monotherapy. The results suggested no increased risk of MACE for phentermine or topiramate users.18
These studies collectively demonstrate that phentermine as monotherapy or in combination with other formulations, contributes to significant weight reduction in diverse populations without causing severe adverse CV effects. The findings underscore the efficacy and tolerability of short-term and long-term phentermine treatment in the management of obesity.9-18
Mital et al conducted an economic evaluation to assess the cost-effectiveness of various AOMs (orlistat, liraglutide, semaglutide (not approved for the management of patients living with obesity in South Africa), and phentermine and topiramate) in the management of adolescent patients living with obesity compared to no treatment. Sensitivity
EPCLUSA® is indicated for the treatment of chronic hepatitis C infection irrespective of genotype in treatment naïve or treatment experienced patients aged 12 years and older and weighing at least 30 kg:
- without cirrhosis or with compensated cirrhosis
- with decompensated cirrhosis in combination with ribavirin 1
Suitable for patients with various levels of liver disease severityb,d 2,3

Proven cure ratec: 98,9 % in real-world analysis2,3
Pan-genotypic and pan-fibroticb,d 3
1 tablet once daily, with or without food, for 12 weeks1
Footnotes: aDespite unknowns in baseline characteristics of some patients, such as: HCV genotype, fibrosis stage, former/current IV drug use, PPI use at baseline and treatment history.3 bA large-cohort international real-world study showed that patients with unknown genotype (n = 42), unknown fibrosis score (n = 82) and unknown treatment history (n = 33) were cured with EPCLUSA® for 12 weeks. Cure is defined as SVR i.e., undetectable HCV RNA after treatment completion.3,4 cCases of HBV reactivation, some of them fatal, have been reported during or after treatment with direct acting antiviral agents including EPCLUSA®. HBV screening should be performed in all patients before initiation of treatment. Treatment with EPCLUSA® should not be initiated in patients who screened positive for hepatitis B virus infection. HBV/HCV coinfected patients are at risk of HBV reactivation, and should therefore be monitored and managed according to current clinical guidelines.1 dPatients with decompensated cirrhosis use EPCLUSA® + ribavirin for 12 weeks.1
Abbreviations: HCV = Hepatitis C Virus; RNA = Ribonucleic acid; IV = Intravenous; PPI = Proton pump inhibitor; SVR = Sustained virological response; HBV = Hepatitis B virus.
References: 1. Epclusa Professional Information approved by the medicine’s regulatory authority. 10 March 2022. 2. Lawitz E, Bourliere M, Han L, McNally J, Stamm LM, Brainard DM, et al. Treatment with SOF/VEL or SOF/VEL/VOX is well tolerated and results in high SVR12 in genotype 1-6 HCV-infected patients with minimal fibrosis: a retrospective analysis of the ASTRAL and POLARIS clinical studies. Poster THU-273 presented at the International Liver Congress 2017, April 19–21, Amsterdam, The Netherlands. Available at: https://www.natap.org/2017/EASL/EASL_07.htm [Accessed 24 March 2022]. 3. Mangia A, Milligan S, Khalili M, Fagiuoli S, Shafran SD, Carrat F, et al. Global real-world evidence of sofosbuvir/ velpatasvir as simple, effective HCV treatment: Analysis of 5552 patients from 12 cohorts. Liver Int 2020;40:1841–1852. 4. National Guidelines for the Management of Viral Hepatitis. Department of Health Republic of South Africa Available at: https://sahivsoc.org/Files/SA%20NDOH_Viral%20Hepatitis%20guideilnes%20final_.pdf [Accessed 10 March 2022]. For full prescribing information refer to the professional information approved by the Medicines Regulatory Authority. S4 EPCLUSA® 400 mg/100 mg film-coated tablets. Reg. No.: 51/20.2.8/0872. Each film-coated tablet contains 400 mg sofosbuvir and 100 mg velpatasvir. Gilead Sciences South Africa (Pty) Ltd., Reg No.: 2014/063761/07, Ground Floor Mac Mac Building, Maxwell Office Park, Magwa Crescent, Waterfall. (Tel: +27 10 346 1920). For any adverse events, please contact: Safety_FC@gilead.com or drugsafetysouthafrica@gilead.com | EPCLUSA®, the EPCLUSA® Logo, GILEAD and the GILEAD Logo are trademarks of Gilead Sciences, Inc. or its related companies. All other trademarks referenced herein are the property of their respective owners. ©2023 Gilead Sciences, Inc. All rights reserved. Date of preparation: 02/2023 | Job code: ZA-EPC-0022
analysis included metformin and two bariatric surgical procedures (sleeve gastrectomy and gastric bypass).19
Results showed that phentermine and topiramate exhibited the highest cost-effectiveness, with an incremental cost-effectiveness ratio of ~R1.7m ($93 620) per quality-adjusted life-year (QALY) relative to no treatment in a simulated cohort of 10 000 adolescents (12- to 17-years) living with severe obesity.19
Orlistat and liraglutide were more expensive and less effective. Bariatric surgical procedures were more effective but were also costlier (~R1.9m to R2.8m [$100 000 to $150 000]) per QALY.19
The global prevalence of obesity poses a significant public health challenge, affecting more than one billion individuals. In South Africa, >50% of adults are overweight or living with obesity, leading to an increased risk of NCDs and premature mortality. Obesityrelated conditions, including T2DM, hypertension, and CVDs contribute significantly to the country’s health burden. Childhood and adolescent obesity are associated with early puberty, menstrual irregularities, and long-term health complications.
The impact of obesity extends beyond physical health. Stigmatisation and discrimination against individuals living with obesity often result in psychiatric disorders such as anxiety, eating disorders, and depression.
Guidelines advocate the use of AOMs for individuals with a BMI of ≥30kg/m². AOMs such as orlistat, phentermine, naltrexone/bupropion, and liraglutide offer diverse mechanisms for weight management.
Phentermine exhibits notable efficacy in weight reduction, as demonstrated by various studies in different populations. Concerns

about CV safety have been addressed, with evidence suggesting that phentermine does not increase the risk of CVDs.
1. World Health Organization. World Obesity Day 2022 – Accelerating action to stop obesity. Updated 2022. [Internet]. Available from: https://www.who. int/news/item/04-03-2022-world-obesity-day-2022-accelerating-actionto-stop-obesity#:~:text=More%20than%201%20billion%20people,they%20 are%20overweight%20or%20obese
2. Boachie M. Obesity costs South Africa billions. We did the sums. 2022. [Internet]. Available from: https://www.wits.ac.za/news/latest-news/opinion/2022/2022-09/ obesity-costs-south-africa-billions-we-did-the-sums.html
3. Goetjes E, Pavlova M, Hongoro C, Groot W. Socioeconomic Inequalities and Obesity in South Africa-A Decomposition Analysis. Int J Environ Res Public Health, 2021.
4. National Department of Health. Strategy for the Prevention and Management of Obesity in South Africa 2023-2028. [Internet]. Available from: https://www. health.gov.za/wp-content/uploads/2023/05/Obesity-Strategy-2023-2028_Final_ Approved.pdf
5. Kokka I, Mourikis I, Bacopoulou F. Psychiatric Disorders and Obesity in Childhood and Adolescence-A Systematic Review of Cross-Sectional Studies. Children (Basel), 2023.
6. Chakhtoura M, Haber R, Ghezzawi M, et al Pharmacotherapy of obesity: an update on the available medications and drugs under investigation. Lancet, 2023.
7. Kim A, Nguyen J, Babaei M, Kim A, et al A Narrative Review: Phentermine and Topiramate for the Treatment of Pediatric Obesity. Adolesc Health Med Ther, 2023.
8. Professional Information. Duromine. Updated 2022. [Internet]. Available at: https://inovapharma.co.za/wp-content/uploads/2022/01/Duromine-PI.pdf
9. Weintraub M, Hasday JD, Mushlin AI, Lockwood DH . A double-blind clinical trial in weight control. Use of fenfluramine and phentermine alone and in combination. Arch Intern Med, 1984.
10. Kim KK, Cho HJ, Kang HC, et al. Effects on weight reduction and safety of shortterm phentermine administration in Korean obese people. Yonsei Med J, 2006.
11. Kang JG, Park CY, Kang JH, et al Randomized controlled trial to investigate the effects of a newly developed formulation of phentermine diffuse-controlled release for obesity. Diabetes Obes Metab, 2010.
12. Kim HO, Lee JA, Suh HW et al Postmarketing Surveillance Study of the Efficacy and Safety of Phentermine in Patients with Obesity. Korean Journal of Family Medicine, 2013.
13. Allison DB, Gadde KM Garvey WT, et al. Controlled-release phentermine/ topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity (Silver Spring), 2012
14. Ryder JR, Kaizer A, Rudser KD, et al. Effect of phentermine on weight reduction in a pediatric weight management clinic. Int J Obes (Lond), 2017.
15. Müller TD, Blüher M, Tschöp MH, et al Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov, 2022.
16. Hendricks EJ, Greenway FL, Westman EC, Gupta AK . Blood pressure and heart rate effects, weight loss and maintenance during long-term phentermine pharmacotherapy for obesity. Obesity (Silver Spring), 2011.
17. Lewis KH, Fischer H, Ard J, et al Safety and Effectiveness of Longer-Term Phentermine Use: Clinical Outcomes from an Electronic Health Record Cohort. Obesity (Silver Spring), 2019.
18. Ritchey ME, Harding A, Hunter S, et al. Cardiovascular Safety During and After Use of Phentermine and Topiramate. J Clin Endocrinol Metab, 2019.
19. Mital S, Nguyen H. Cost-Effectiveness of Antiobesity Drugs for Adolescents With Severe Obesity. JAMA Netw Open, 2023. SF

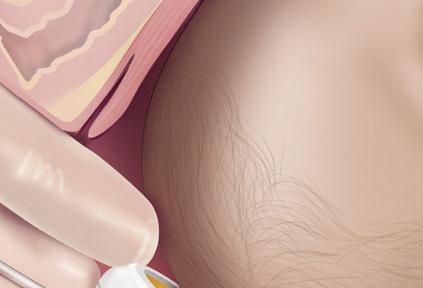
Operative vaginal delivery, involving the use of vacuum-assisted delivery (VAD) systems, is a crucial skill in obstetric care and is used to expedite the birthing process. This technique, alongside forceps deliveries, offers obstetricians the flexibility to opt for a more personalised approach to delivering babies, based on clinical judgment and patient-specific factors.1

Operative vaginal deliveries are classified based on the status of the foetal head and the degree of rotation needed. These classifications include outlet delivery, low delivery, and mid delivery, each defined by specific foetal head positions and rotations during the extraction process.1
The use of VAD is contraindicated in certain foetal conditions, such as bleeding disorders and demineralising diseases. Additionally, the procedure is discouraged before 34 weeks of gestational age. Obstetricians must ensure that all prerequisites are met and the patient consents to the care plan before proceeding.1
The use of VAD is considered
‘appropriate’ in certain circumstances such as maternal exhaustion, non-reassuring foetal heart rate, prolonged second stage of labour, or specific maternal conditions.1 Prerequisites include a fully dilated cervix, previously ruptured membranes, engagement of the foetal head, known head position, foetal weight estimation, adequate pelvic dimensions, adequate anaesthesia (often an epidural), the maternal bladder has been emptied, and the patient’s agreement after informed consent.1
A backup plan (typically a caesarean section) should be in case of failure, recommends Tonismae et al.
According to the authors, VAD systems, are often preferred over forceps. These systems come in various designs, with soft-cup devices minimising neonatal scalp injuries. One of the most popular is the Kiwi Complete Vacuum Delivery System.1,2
Tonismae et al stress that adequate training is crucial when using a VAD system to minimise complications. An operator and at least one assistant should be present, with additional personnel available for infant resuscitation if required.1
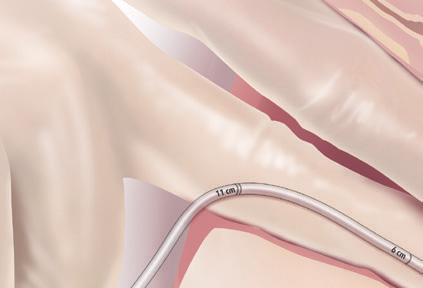
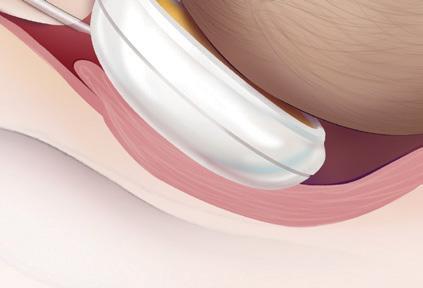
The technique involves careful application of the vacuum cup to the foetal
scalp, ensuring proper placement for flexion, descent, and rotation of the vertex during traction (see below).1
The procedure requires skilled monitoring and coordination, and suction is applied during contractions. Multiple detachments are discouraged, with caesarean section considered if detachment occurs more than two to three times.1
Maternal and newborn complications that indicate vacuumassisted delivery is needed
Maternal complications may include vaginal lacerations and pain, while newborn complications may range from scalp lacerations to intracranial haemorrhage. Although complications are generally rare, practitioners should be vigilant and prepared for potential adverse outcomes.1
Continuous re-evaluation during the delivery process is essential, with a focus on avoiding rocking motions and excessive torque. The maximum time for vacuum delivery and the acceptable number of detachments remain uncertain, but recommendations suggest limiting vacuum application time to 20-30 minutes and restricting detachments to two to three.1
Tonismae et al emphasise optimal cup placement over the foetal head flexion point, intermittent suction application, and careful consideration of vacuum application time and number of pulls. Traction should follow the pelvic curve to maintain foetal head flexion, with adjustments as the head descends.1
The crucial initial step in the VAD process involves identifying the correct attachment point on the baby’s scalp, located 3cm anterior to the posterior fontanelle along the midline of the sagittal suture. 3
The VAD device is then applied to create a secure attachment using vacuum pressure, resulting in the formation of a fluid-filled elevated region on the scalp known as the caput succedaneum chignon. This localised oedema, induced by the vacuum, serves as a mechanical interface between the scalp and the device. 3
The formation of the chignon enables the clinician to use the VAD handle during contractions to assist the mother by promoting descent through the birth canal. This process is especially beneficial when the foetal head is malpositioned, as the correctly positioned VAD induces flexion and descent, facilitating spontaneous rotation to the ideal occiput anterior position. 3
The clinician should carefully monitor the baby’s position and employ counter-traction if needed to maintain device position during traction. Traction is a two-handed exercise,
with one hand preventing cup tilting and the other monitoring descent without the bony skull moving, indicating an obstruction. This technique aids in gauging and regulating tractive force, crucial during outlet deliveries.3
The entire procedure typically lasts around 10 minutes with two to three pulls, exerting forces up to 115N. The success rate exceeds 80% when using a commonly available VAD device like the Kiwi, according to Goordyal et al 3
The device remains in use until the baby’s head crowns, representing the most significant resistance. The vacuum is released after the foetal chin emerges from the introitus. 3
In some cases, VAD may be required for rotational delivery, involving a redirection of traction according to the station of delivery and along the axis of the maternal pelvis. 3
VAD can be used in cases such as maternal exhaustion, nonreassuring foetal heart rate, or prolonged second stage of labour
Patient counselling is essential Effective communication with patients is crucial, allowing time for counselling on the purpose, procedure, hazards, and alternatives. The discussion should also address potential outcomes if the vacuum procedure fails, considering cesarean delivery as an option.1
Conflicting data on the impact of failed vacuum assistance on cesarean outcomes necessitate careful consideration and transparent communication with expecting parents.1
Benefits of the Kiwi system compared to conventional vacuum delivery
Siggelkow et al compared the safety and efficacy of the Kiwi OmniCup system with conventional vacuum delivery by examining completed births, drop-off rates, and various secondary outcome measures for both instruments. 5
The retrospective study included 4682 births, with 217 undergoing operative vaginal deliveries (4.6%). Of these, 79 used conventional vacuum extraction (37%) and 138 utilised the Kiwi system (63%). 5
The Kiwi OmniCup, a single-use instrument with an integrated hand pump, features a flexible suction and traction element designed for ease of insertion centrally. 5
Lateral traction leads the traction element into a groove, facilitating rotation of the head, especially in anterior and posterior cephalic presentations. 5
Results indicated that the use of the Kiwi system led to a significant reduction in episiotomies compared to the control group (61% vs 76%).
Despite the higher incidence of cup detachment with the Kiwi system, the study found similar rates of maternal and foetal injuries for both systems. 5
Bodner-Adler et al aimed to assess the correlation between mediolateral episiotomy and severe perineal trauma during Kiwi vacuum deliveries in nulliparous women. 6
Analysing 572 cases from 2010 to 2015, the study found a 96% success rate in completing births with a 4% failure rate. Among the subjects, 65% underwent Kiwi vacuum delivery with episiotomy. 6
The occurrence of third- or fourthdegree perineal tears was 6.6%, and it was significantly lower in women with Kiwi vacuum deliveries combined with episiotomy. 6
Additionally, the rates of perineal tears of all degrees, vaginal tears, and labial trauma were significantly reduced when Kiwi vacuum delivery was accompanied by mediolateral episiotomy. 6
This suggests that performing a mediolateral episiotomy is associated with a decreased risk of severe perineal tears and other genital tract trauma in Kiwi vacuum deliveries. 6
Operative vaginal delivery, particularly with VAD systems like the Kiwi system, plays a crucial role in obstetric care. Personalised approaches to operative vaginal delivery should be based on clinical judgment and patient-specific factors.
The Kiwi system, with its soft cup design and unique features, proves advantageous over conventional vacuum delivery, significantly reducing episiotomies. Additional studies highlight the benefits of Kiwi vacuum deliveries with mediolateral episiotomy, showing significantly lower rates of severe perineal tears and genital tract trauma.
Effective patient communication and proper training are essential for successful VAD procedures, establishing it as a viable alternative to cesarean section with fewer complications in well-trained hands.
References are available on request. SF






















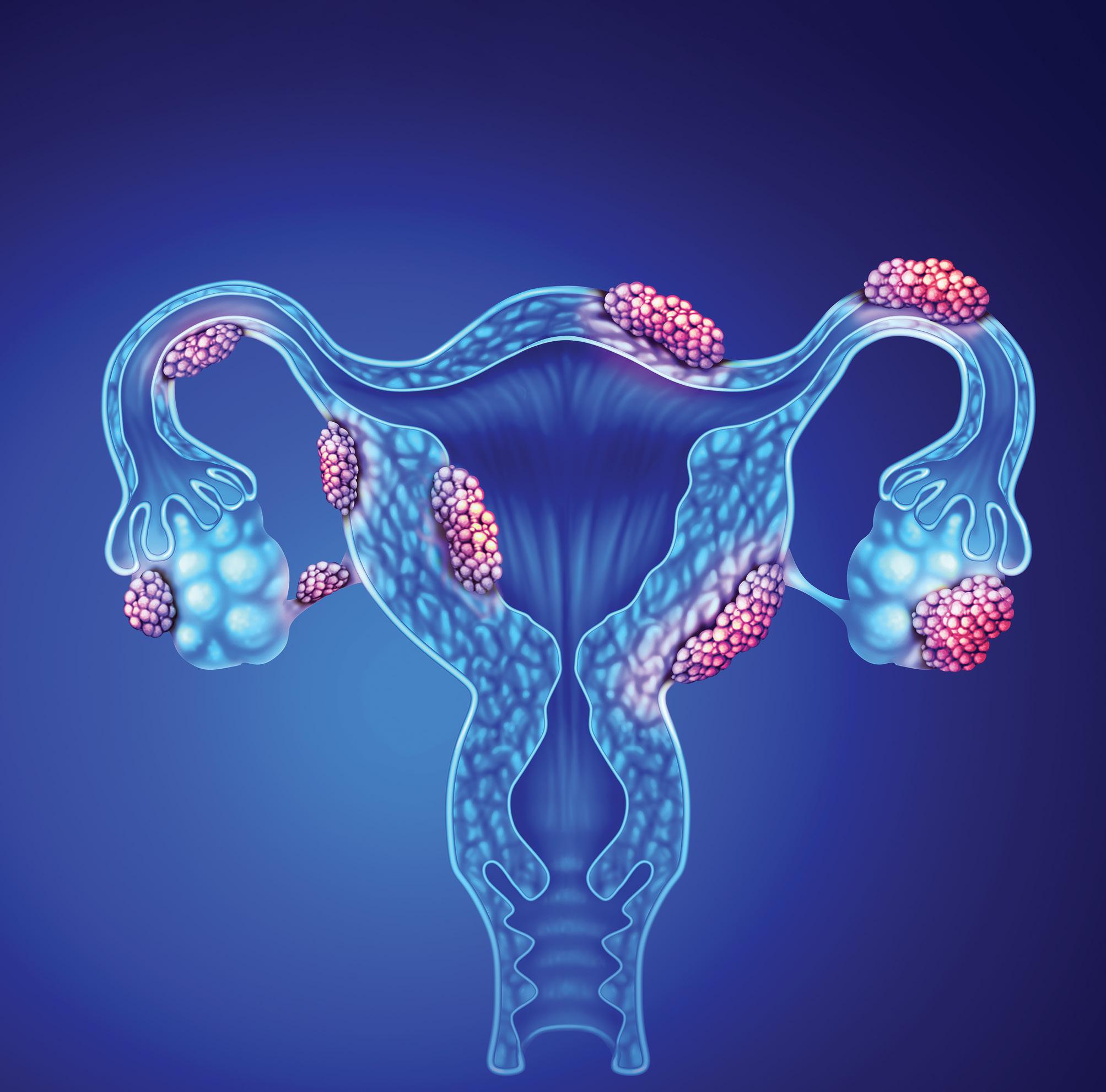
Endometriosis, one of the main reason why couples consult reproductive specialists, is a misunderstood disease, shrouded in mystery as a result of misinformation and taboos, which significantly affects various aspects of women’s lives, including fertility, sexuality, work, and relationships.1
In her article entitled The Puzzle of Endometriosis, Ballweg quotes a colleague who describes endometriosis as ‘a riddle, wrapped in a mystery inside an enigma’. 2 In the decades following the publication of her article, it seems as though little has changed, and endometriosis is still a misunderstood disease.
Endometriosis affects ~10% of women of reproductive age and is the cause of between 35% and 50% of infertility. The main symptoms include intense dysmenorrhea (severe and frequent menstrual cramps and pain during menses), dyspareunia (persistent or recurrent genital pain that occurs just before, during or after intercourse) and chronic pelvic pain. It takes on average seven years before a diagnosis is confirmed.1
Endometriosis is characterised by the development and presence of histological elements like endometrial glands and stroma in anatomical positions and organs outside of the uterine cavity. 3
Gremillet et al recently published the findings of their qualitative study, which explored the impact of severe endometriosis on the professional lives of women living with infertility.1
Pain is the most prominent symptom, hindering work and leading to a substantial reduction in effective work hours. Digestive and urinary problems, along with heavy bleeding, contribute
to frequent work interruptions. The cyclical and unpredictable nature of symptoms causes difficulty in concentration, chronic fatigue, anxiety, and irritability.1
Many women choose not to disclose these challenges to employers and colleagues due to fear of judgment and negative reactions. Privacy preservation, better information dissemination, and self-protection are key motivators for those who do decide to share their experiences.1
Often, such revelations are made discreetly during off-the-record meetings with superiors, with women feeling it more legitimate to justify absences by medicalising their infertility.1
This disclosure is seen as a pivotal moment in their professional lives, fostering understanding and support from their























Start

















































2 mg dienogest / film-coated tablet



professional environment, ultimately making work more manageable.1
A definitive diagnosis of endometriosis is mainly based on surgical findings. Dependence on symptoms that require surgery, may be at the root of delayed diagnosis in many cases. 4
Early diagnosis is vital to protect fertility, especially in light of the impact of age on ovarian reserve (the reproductive potential left within a woman’s two ovaries based on number and quality of eggs). 4
Understanding the pathogenesis of endometriosis plays a crucial role in decisions regarding clinical and therapeutic interventions. Some of the most popular theories regarding the pathogenesis of endometriosis include:4
_ The retrograde menstruation theory, proposed by Sampson in 1927, suggests that viable endometrial tissue moves into the pelvic cavity during menstruation, adheres to peritoneal cells, and invades structures, explaining endometriosis.
Early menses onset, heavy menstrual flow, and anatomical predominance on the right side support this theory.
_ The coelomic metaplasia and mullerian remnants hypotheses propose in situ origin from embryological remnants.
_ Sampson’s hematogenous and lymphovascular dissemination theory suggests endometrial cell spread via vasculature, supported by murine models and clinical evidence of emboli in lymph nodes.
_ The stem cell theory posits altered stem cell trafficking as key to endometriosis. Bone marrow-derived stem cells contribute to endometrial regeneration, with increased pluripotential cells in women with endometriosis during menses. These cells can differentiate into endometrial cells outside the uterus, explaining extraperitoneal endometriosis.
_ Genetic factors contribute, with familial clustering and heritability estimated at 51%. Genome-wide studies link endometriosis to risk loci in sex steroid hormone pathways. In infertility, folliclestimulating hormone beta (FSHB) and follicle-stimulating hormone receptor (FSHR variants impact hormonal profiles. FSHB and FSHR are genes associated with the production and regulation of follicle-stimulating hormone (FSH), a key hormone in the reproductive system.
_ The epigenetic theory emphasises dynamic changes in chromatin structure. DNA methylation, especially in genes like homeobox gene10 (HOXA10), essential
for unravelling the molecular mechanisms that govern embryonic development and for gaining insights into the origins of various congenital disorders, has been linked to impaired uterine receptivity. Aberrant DNA methylation in progesterone receptor genes contributes to persistent progesterone resistance. Histone modifications, such as hypoacetylation, occur in endometriotic stromal cells. Over 100 microRNAs are expressed in endometriotic lesions, influencing processes like epithelialmesenchymal transition, cell proliferation, and angiogenesis. Epigenetic factors may offer diagnostic, prognostic, and therapeutic insights into endometriosis. However, according to Bonavina et al, these theories do not explain the natural history of the disease.4
Pain plays a crucial role in endometriosisrelated infertility, affecting the possibility of intercourse
Pain and mechanical factors
Pain plays a crucial role in endometriosisrelated infertility, affecting the possibility of intercourse. Superficial and deep dyspareunia make intercourse difficult, leading to avoidance, thus impacting conception.4 Endometriosis, particularly in severe stages, increases the risk of deep dyspareunia by nine-fold due to its effect on pelvic structures. Furthermore, endometriosis-associated pelvic pain can reduce sexual desire, and arousal. Mechanical factors like pelvic adhesions and anatomical distortion further hamper conception.4
Ovarian reserve, a key fertility prognostic factor, is adversely affected by endometriosis, particularly in endometriomas. Ovarian reserve lacks precise predictive tools, but antral follicle count and anti-Mullerian hormone levels are widely used to determine a women’s reproductive potential. 4
Endometriomas (unique cysts with no real
capsule) exchange contents with the healthy ovarian cortex, inducing oxidative stress, inflammation, and fibrosis. Histopathological studies reveal reduced follicular numbers and activity in endometriomas.4
The impact of endometriosis on oocyte quality, which is crucial for fertility preservation, is much debated. While some studies show no impact on embryo morphology, others using time-lapse technology suggest altered relative kinetics, indicating poorer embryo quality. 4
Dysregulation of steroidogenesis change the follicular microenvironment, and oxidative stress in granulosa cells contribute to reduced oocyte quality. Furthermore, follicular fluid from endometriosis patients induces DNA damage in oocytes and systemic and peritoneal inflammation in endometriosis influences follicular fluid composition and damages spindle and chromosomes in oocytes.4
Gamete transport, anatomical distortions, and inflammatory microenvironments associated with endometriosis impair sperm-oocyte interaction and disrupt acrosome reactions.4
Clinical data on spontaneous ovulation rates in women living with endometriosis are limited and contentious. Elevated prolactin levels, significantly present in these women, may contribute to anovulation by disrupting luteinizing hormone pulsatility and hindering hypothalamic function. 4
Hyperprolactinaemia (elevated levels of prolactin, a hormone produced by the pituitary gland) inhibits oestrogen receptors, inhibiting ovulation. Luteinized unruptured follicle syndrome, a condition characterised by the failure of a mature ovarian follicle to release its egg (ovulate) during the menstrual cycle, even though the follicle has undergone the luteinization process, forming a structure called a corpus luteum, is another potential cause of ovulation failure. 4
Women living with endometriosis may also experience altered oestrogen and progesterone patterns, compromising the luteal phase (a specific stage of the menstrual cycle that occurs after ovulation and before the onset of menstruation) and hindering ovulation. 4
Women living with endometriosis experience reduced implantation rates in natural and assisted reproductive cycles, indicating
potential defects in endometrial receptivity. The eutopic endometrium exhibits molecular and functional abnormalities.4
Furthermore, dysregulation of steroid hormone signalling, progesterone resistance, and altered hormone receptor levels contribute to impaired endometrial receptivity. 4
Histological criteria for assessing receptivity have limitations, prompting a shift to molecular analyses. Dysregulated genes, including HOXA10 and integrins, crucial for implantation, exhibit altered expression in endometriosis. 4
Defects in decidualisation, immune cell imbalances, and pro-inflammatory conditions further contribute to an unfavourable environment for embryo implantation.4
Adenomyosis and other uterine factors
Endometriosis frequently coexists with adenomyosis (characterised by the presence of endometrial tissue, which normally lines the uterus, growing into the muscular wall of the uterus (myometrium), especially in infertile women, and their concomitant presence may worsen fertility outcomes.4
Meta-analyses show that women with adenomyosis have lower clinical pregnancy rates, higher miscarriage risks following assisted reproductive technology (ART), and adverse pregnancy outcomes. 4
How do you manage endometriosisassociated infertility?
Endometriosis currently lacks a curative treatment. Clinical management of endometriosis-associated infertility is challenging due to diverse patient phenotypes, requiring a personalised approach. Pharmacotherapy and surgical interventions are aimed at managing symptoms. 4,5
Pharmacotherapy aims to reduce inflammation, suppress ovarian cycles, and inhibit oestrogen effects. Surgery may involve removing identified endometriotic lesions or complete excision of pelvic organs. Treatment decisions should be based on factors like age, ovarian reserve, infertility duration, and concomitant factors.4,5
Pharmacotherapy options include hormonal therapies inducing a hypoestrogenic state (oral contraceptives, progestins, danazol, gonadotropin hormone-releasing hormone [GnRH] agonists), as well as pain-relieving agents like nonsteroidal anti-inflammatories (NSAIDs) and opioids. 5
The European Society of Human Reproduction and Embryology (ESHRE) endometriosis guideline suggests offering
hormone treatment or surgery for recurrent pain in women living with endometriosis. 6
Pharmacotherapy options include NSAIDs, hormone treatments (combined hormonal contraceptives, progestogens, GnRH agonists, or antagonists), and others. Shared decision-making is encouraged, considering individual factors like preferences, side effects, efficacy, costs, and availability.6
Surgical management options involve cystectomy instead of drainage and coagulation for ovarian endometriomas, minimising ovarian damage. Reproductive surgery can improve pregnancy rates in stages I/II endometriosis (see Table 1). 4,6,7
Stage Classification Description
I Minimal A few superficial implants
II Mild More and slightly deeper implants
III Moderate Many deep implants, small endometriomas on one or both ovaries, and some filmy adhesions
IV Severe Many deep implants, large endometriomas on one or both ovaries, and many dense adhesions, sometimes with the rectum adhering to the back of the uterus
Advanced stages (III/IV), especially deep infiltrating endometriosis (DIE), present complexities. The role of surgery in DIErelated infertility lacks strong evidence, and risks must be weighed. 4
Hysterectomy (with or without ovary removal) is an option for those not seeking conception, but its efficacy is not guaranteed. Postoperative use of levonorgestrel-releasing intrauterine system or combined hormonal contraceptives may be recommended for secondary prevention. 6
For women living with endometriomas, clinicians should consider ovarian cystectomy instead of drainage and electrocoagulation, weighing the risk of reduced ovarian reserve. 6
Post-operative hormone treatment (eg combined hormonal contraceptives) is suggested for long-term prevention of symptom recurrence. 6
Regarding alternative options, ESHRE recommends non-medical strategies to address the quality of life (QoL) and psychological well-being of women living with endometriosis. However, no specific non-medical intervention is recommended
for pain reduction or improvement in QoL, as their potential benefits and harms remain unclear. 6
Fertility preservation is essential in endometriosis, and options include embryo, oocyte or ovarian tissue cryopreservation. Vitrification technology for oocyte cryopreservation has shown superior clinical outcomes compared to traditional slow-freezing methods. 4
While embryo and oocyte cryopreservation are considered nonexperimental, the strength of evidence supporting fertility preservation in endometriosis is limited. 4
Subgroups, particularly those with bilateral endometriomas or contralateral recurrence after surgery, might benefit from fertility preservation. Ovarian tissue cryopreservation is an alternative, especially when ovarian hyperstimulation is contraindicated.4
The impact of endometriosis on women’s fertility is intricate and multi-faceted, requiring a comprehensive understanding of its pathogenesis, pathophysiology, and effective clinical management strategies.
The journey towards fertility preservation for women living with endometriosis involves addressing not only the physical symptoms but also the emotional and professional challenges women face.
1. Gremillet L, Netter A, Sari-Minodier I, et al Endometriosis, infertility and occupational life: women’s plea for recognition. BMC Women’s Health, 2023.
2. Ballweg ML. The Puzzle of Endometriosis. In Endometriosis, edited by CR Nezhat, GS Berger, FR Nezhat, VC Buttram, and CH Nezhat. New York, NY: Springer, 1995.
3. Monnin N, Fattet AJ, Koscinski I. Endometriosis: Update of Pathophysiology, (Epi) Genetic and Environmental Involvement. Biomedicines, 2023.
4. Bonavina G, Taylor HS. Endometriosisassociated infertility: From pathophysiology to tailored treatment. Front Endocrinol, 2022.
5. Della Corte L, Di Filippo C, Gabrielli O, et al The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int J Environ Res Public Health, 2020.
6. Becker CM, Bokor A, Heikinheimo O, et al ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum Reprod Open, 2022.
7. MSD Professional Version. Stages of Endometriosis. [Internet]. Available at: https:// www.msdmanuals.com/professional/multimedia/ table/stages-of-endometriosis SF

Specialist Forum recently hosted a webinar entitled Cervical cancer prevention with CERVARIX, an adjuvanted human papillomavirus (HPV) vaccine designed to prevent cervical cancer (CxCa). The webinar was presented by Dr Olakunle Oladehin, Area Medical Lead, Emerging Markets, GSK Vaccines.
Key Points from the webinar
Persistent HPV infection:
_ The transition from persistent HPV infection to invasive carcinoma can take several years.
_ There are over 130 HPV subtypes, with 15 classified as oncogenic. HPV-16 and HPV18 are the most common, accounting for over 70% of invasive CxCa cases.
Cervarix targets HPV types 16 and 18:
_ Cervarix is a bivalent vaccine containing viral-like particles (VLPs) of HPV 16 and 18.
_ It provides protection against precancerous cervical lesions associated with non-vaccine oncogenic HPV types like HPV-31 and HPV-45.
Importance of sustained protection:
_ Cervarix contains an adjuvant system (AS04) with aluminium hydroxide and monophosphoryl lipid A (a tolllike receptor 4 agonist). Adjuvanted formulations show a high and sustained immune response over time, while non-adjuvanted ones elicit a
weaker and quickly waning response. Immunostimulants further boost the overall efficacy.
_ Clinical studies, including Efficacy Study of HPV-16/18 Vaccine (GSK 580299) to Prevent HPV-16 and/or -18 Cervical Infection in Young Healthy Women (HPV- 001), demonstrate strong and sustained immune responses in young girls over ten years.
_ Mathematical models project that adjuvanted Cervarix can offer sustained protection for over 50 years.
_ Follow-up studies, such as the Follow-up Study of GSK Biologicals’ Human Papilloma Virus (HPV) Vaccine to Prevent Cervical Infection in Young Adults (HPV 007) and the Follow-up Study to Evaluate the Long-term Efficacy of the HPV Vaccine (580299) in Healthy Young Adult Women in Brazil (HPV 023), affirm Cervarix’ s sustained protection >10 years and indicate potential protection for >50 years.
_ Cervarix consistently demonstrates efficacy against various stages, including
persistent infection and cervical intraepithelial neoplasia.
Real-world evidence:
_ Evidence from the United Kingdom, Scotland, and South Africa highlights substantial reductions in CxCa and highgrade lesions, emphasising the vaccine’s impact and potential economic benefits.
_ Safety analyses in males show a comparable safety profile to the hepatitis B vaccine, with continuous monitoring for emerging risks.
Cervarix, through its carefully formulated adjuvanted system, has demonstrated efficacy in providing sustained protection against HPV-related diseases, particularly CxCa. Real-world evidence supports its positive impact on reducing disease burden and healthcare resource utilisation.
To view the replay video, go to Medical Academic and click on the webinar/ events bar or go to: https://vimeo.com/ event/4077869 SF
This article was independently sourced by Specialist Forum.
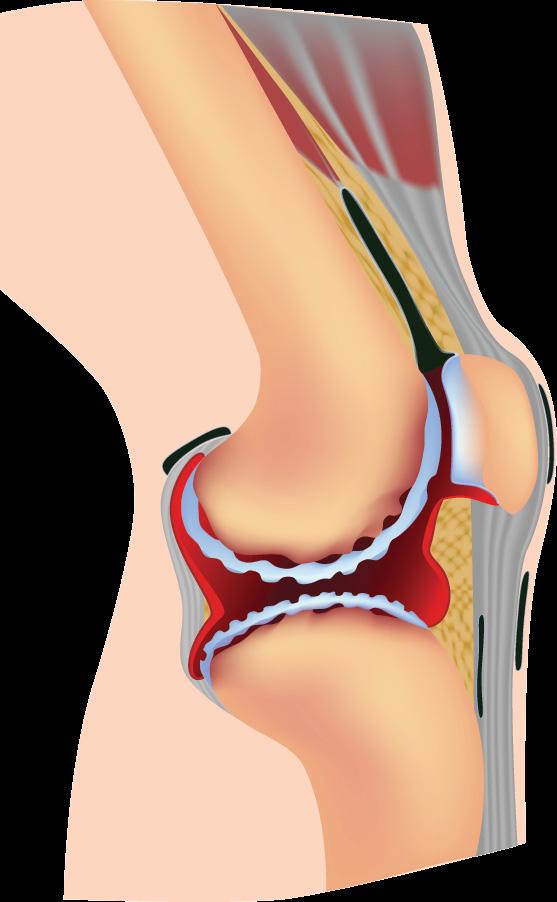
Rheumatoid arthritis (RA) is a common autoimmune disease characterised by a progressive inflammatory synovitis of the joints, leading to cartilage and bone damage as well as disability. Over the past two decades, the implementation of the treat-totarget (T2T) strategy in the management of patients living with RA and treated with disease-modifying anti-rheumatic drugs (DMARDs) have revolutionised the management of the disease.1,2
his strategy involves establishing a specific treatment target, such as achieving remission or maintaining low disease activity (LDA), and employing rigorous control measures, including regular monthly assessments and corresponding adjustments to treatment, to attain this predefined target. 2
The strategy typically adheres to a structured protocol for modifying treatments based on the level of disease activity and the response to the ongoing treatment. 2
Clinical remission in patients with RA is characterised by the absence of signs and symptoms indicating significant inflammation. Remission can be determined using various instruments, such as the Disease Activity Score (DAS) with 28-Joint Count, the Clinical Disease Activity Index (CDAI), and Simplified Disease Activity Index (SDAI) and the Boolean remission criteria. 3
The DAS assigns a numerical score ranging from 0 to 10, with a higher score indicating a higher level of disease activity. When evaluating treatment response, a reduction of 0.6 in DAS-28 signifies a moderate improvement, whereas a reduction >1.2 reflects a significant improvement.4
A DAS-28 score <2.6 suggests the achievement of disease remission, a score of between 2.6-3.2 suggests LDA, a score of >3.2-5.1 suggests moderate disease activity and >5.1 suggest high disease activity.4
Both the American College of Rheumatology (ACR) and the European Alliance of Associations for Rheumatology (EULAR) proposed the following two sets of remission criteria: the Boolean criteria (the fulfilment of the four core set measures of
tender joint count of ≤1, swollen joint count of ≤1, C-reactive protein of ≤1mg/dl, and patient global assessment score of ≤1) and the SDAI-based criteria (an SDAI score of ≤3.3), to which the CDAI-based criteria (a CDAI score of ≤2.8) were considered equivalent in clinical practice. 5
Although achieving and maintaining remission is considered the ideal treatment goal in RA, it is challenging to achieve. For instance, reports indicate that sustaining remission in early RA over a 10-year period, based on various disease activity criteria, is achieved by <50% of patients. In contrast, attaining LDA, which is a less stringent outcome criterion, proves to be more feasible in routine clinical practice. 6
Apart from conventional synthetic DMARDs such as methotrexate, leflunomide, and sulfasalazine, other treatment options available include biological DMARDs (bDMARDs), targeted synthetic DMARDs (tsDMARDs), non-steroidal anti-inflammatory drugs (NSAIDs), and glucocorticoids (GCs).1,7
Conventional DMARDs are the initial recommended treatment for RA. In instances where first-line treatments prove ineffective, the next line of therapeutic options includes bDMARDs, such as tumour necrosis factor inhibitors, anti-interleuken-6 agents, T-cell activation blockade, or tsDMARDs such as Janus kinase inhibitors (JAKis).1
The updated EULAR guidelines recommend the following:7
1 Treatment should aim to achieve sustained remission or LDA in every patient.
2 DMARD therapy should be initiated as soon as the diagnosis of RA is confirmed. Management should focus on those with a compelling clinical diagnosis of RA.
3 Frequent monitoring (every one to three months) is recommended in active disease. If there is no improvement within three months of treatment initiation or the target is not reached within six months, therapy should be adjusted.
4 MTX should be part of the first treatment strategy. Although hydroxychloroquine is not explicitly recommended, it may be used in patients with early, mild disease when the other csDMARDs are contraindicated or not tolerated.
5 In cases where MTX is contraindicated or patients exhibit early intolerance, leflunomide or sulfasalazine should be considered as part of the first treatment strategy.
6 Short-term GCs (no more than three months) should be considered when initiating or changing conventional DMARDs, with different dose regimens and routes of administration.
7 csDMARDs, leflunomide, and sulfasalazine can be considered for patients in whom MTX is contraindicated or intolerant to methotrexate (MTX) may consider leflunomide or sulfasalazine as part of the first treatment strategy.
8 When the first csDMARD strategy fails to achieve the treatment target, the addition of a bDMARD is recommended, and JAKis can
be considered for certain patients considering individual risk factors and after discussion with patients.
9 The EULAR Task Force supports the combination of bDMARDs and tsDMARDs with conventional DMARDs. MTX continuation is recommended, and the possibility of reducing MTX dosage to 10mg weekly is recommended for enhanced benefits.
10 Considering another bDMARD or tsDMARD if the initial treatment fails. The update incorporates evidence supporting the interchangeability of IL-6 receptor inhibitors.
11 Consider dose reduction after sustained remission. The order of tapering bDMARDs and csDMARDs is left to the discretion of patients and rheumatologists. Avoiding complete cessation and opting for dose reduction or interval increase is important.
How effective is the T2T strategy?
The implementation of the T2T strategy has significantly improved the prognosis of patients living with RA. Both EULAR and the ACR recommendations have embraced the T2T strategy as a central element in the management of RA.7,8
According to the ACR guideline, a T2T strategy is strongly advised for patients initiating treatment with bDMARDs or tsDMARDs. This approach involves optimising MTX dosage and incorporating additional DMARDs when necessary. 8
According to the authors of the ACR guideline, the recommendation is based on low certainty evidence, but the recommendation is robust due to the acknowledged significance of systematic monitoring and treatment adjustments. The goal is to minimise inflammation, preventing joint damage, cardiovascular disease, and osteoporosis in the long term. 8
For patients with an insufficient response to bDMARDs or tsDMARDs, a T2T strategy is conditionally recommended over usual care. Usual care involves treatment adjustments based on shared decision-making. 8
The recommendation is conditional, given uncertain incremental benefits in this patient population. Factors influencing this decision include the number of available treatment options, the impact of non-inflammatory causes on disease assessments, and the patient’s threshold for changing medications.8
The ACR conditionally recommends a minimal initial treatment goal of LDA over aiming for remission, while EULAR recommends remission as the main treatment goal. The ACR’s recommendation is based on the fact that achieving remission
may be challenging for many patients.8
However, state the authors of the ACR guidelines, remission is a reasonable initial goal for those with early disease and minimal exposure to bDMARDs and tsDMARDs. The flexibility of reassessing treatment goals over time and considering individual patient preferences is crucial to ensure personalised care. 8
Recent real-world studies have consistently confirmed higher remission rates and improved quality of life (QoL) in patients following the T2T strategy compared to those receiving usual care.9,10
Xie et al investigated trends in RA activity and assess the effectiveness of the T2T strategy in routine clinical practice. Medical records of patients (n=1001) living with RA from 2009 to 2016 were systematically reviewed. Disease activity score were assessed using DAS28, SDAI, and CDAI during clinic visits.9
Mean and time-adjusted methods were applied to calculate annual disease activity and remission rates. A comparison of disease activity and remission rates was made before and after the initiation of the T2T strategy in 2011.9
Additionally, a sub-cohort study, comprising T2T and non-T2T groups, examined cumulative remission percentages and time to achieve first remission during the first-year follow-up.9
The researchers observed significant improvements in disease activity and remission rates, as measured by all four indices over the eight-year period. Following T2T adherence in 2011, a higher proportion of patients achieved LDA, and increased remission rates compared to the years 2009 and 2010.9
The sub-cohort analysis showed that more patients (49.3%-73.2% vs 19.1%-34.5%) achieved remission with a shorter median time compared to the non-T2T period group, particularly in DAS28-CRP (21 vs >52 weeks) and DAS28-ESR (37 vs >52 weeks).9
Brinkmann et al investigated the twoyear impact on disease activity and healthrelated QoL (HRQoL) resulting from the implementation of a clinical practice T2T strategy in patients living with RA.10
Patients enrolled in the Norwegian Very Early Arthritis Cohort 2.0, spanning from 2010 to 2015, received treatment based on T2T principles, involving scheduled visits at baseline, three, six, nine, and 12 months, followed by visits every six months and monthly assessments until achieving a DAS28 score of <2.6.10
This T2T cohort was compared with
a pre-T2T group of patients included in the Norwegian-DMARD register from 2006 to 2009. Both cohorts were clinically diagnosed with RA (≤1-year) and were treatment-naive for DMARDs. Disease activity and HRQoL outcomes were analysed, with the primary endpoint being SDAI remission (≤3.3) at two years.10
At the two-year mark, 46% of patients in the T2T cohort achieved SDAI remission, compared to 31% in the routine care cohort. Although EuroQol-5 Dimension, a standardised instrument for measuring HQRQoL, scores were similar at baseline, they significantly differed between groups at two years (0.77 vs 0.73).10
Huang et al analysed data from the Collaboratively intENsive Treat-to-target in RA (CENTRA) and Treat-to-TARget in RA (TARRA) cohorts. TARRA, an observational study, focused on ‘casual control’, while CENTRA, a prospective cohort, adhered to a collaboratively tight-control T2T strategy. Using 1:3 propensity score matching, patients in both cohorts were compared, with the primary outcome being the SDAI at 12 months.11
In the TARRA study, usual care was provided by a rheumatology, no fixed appointments were scheduled, only DAS scores were calculated, and patients were provided with limited education.11
In the CENTRA study, patients were treated by a team of rheumatologists as well as a specially trained nurse. Followups were scheduled every three months during the first 12 months and then every six months after the patients achieved either remission or LDA. Apart from DAS scores, additional assessments were performed, and patients underwent two educational session per annum.11
Patients from CENTRA (enrolled between 2015 and 2019) and those from TARRA (enrolled between 2009 and 2015) were included after an exclusionary process. Demographic factors such as age, gender, disease course, and seropositivity were similar in both groups.11
MTX was the most commonly used medication in both TARRA and CENTRA (81.2% vs 85.3%, respectively), with a higher percentage of TARRA patients receiving GCs (49.1% vs 24.5%, respectively).11
The CENTRA cohort exhibited significantly lower SDAI scores compared to the TARRA cohort (2.1 vs 3.4). CENTRA patients also showed better CDAI and DAS-28 measurements at months three, six, and 24 compared to the TARRA cohort.
More CENTRA group patients achieved SDAI-defined remission compared to the TARRA cohort (70.6% vs 49.4%).11
What are some of the challenges in implementing a T2T strategy?
According to Ford et al, shared decisionmaking between the treating physician and patient, adherence to treatment and frequent follow-up are essential for the successful implementation of a T2T strategy.12
Shared decision-making involves a comprehensive discussion of preferences, risks, and benefits regarding treatment goals and changes. It is pivotal for the treating physicians to provide patients with relevant and evidence-based information to ensure a reasonable level of patient understanding to allow them to make informed decisions.12
Despite guidelines supporting universal DMARD use, a systematic review revealed that only 30%-73% of patients living with RA in non-rheumatology care are prescribed DMARDs.12
Access to rheumatologists is limited, particularly in rural areas, exacerbating the issue. The discomfort of non-rheumatologists in managing RA contributes to this problem, as they may lack education on RA and familiarity with DMARDs.12
Physician factors further complicate T2T implementation. Even under rheumatologist care, patients living with RA may not receive timely treatment changes.12
Qualitative interviews with rheumatologists revealed a discrepancy between their perception of T2T engagement and actual practice. Some physicians may resist T2T due to a perceived reduction in autonomy and devaluation of their clinical expertise.12
Patient factors, such as satisfaction with current disease control and fear of treatment side effects, impact willingness to escalate therapy. Studies indicate that patients may be satisfied despite moderate or high disease activity. Patient inertia include fear of medications and denial of sick identity, while motivations to accept treatment include a desire to return to normal life.12
As mentioned, adherence to prescribed therapies is essential for T2T success. Studies demonstrate varying adherence rates among patients living with RA, indicating room for improvement in ensuring patients stick to their treatment plans.12
Systemic issues within the healthcare system present additional challenges. Frequent visits may strain patient resources, and rheumatologists’ schedules. Time constraints, insurance approval delays for DMARDs, and the lack of systemic incorporation of disease activity measures further hinder effective T2T implementation.12
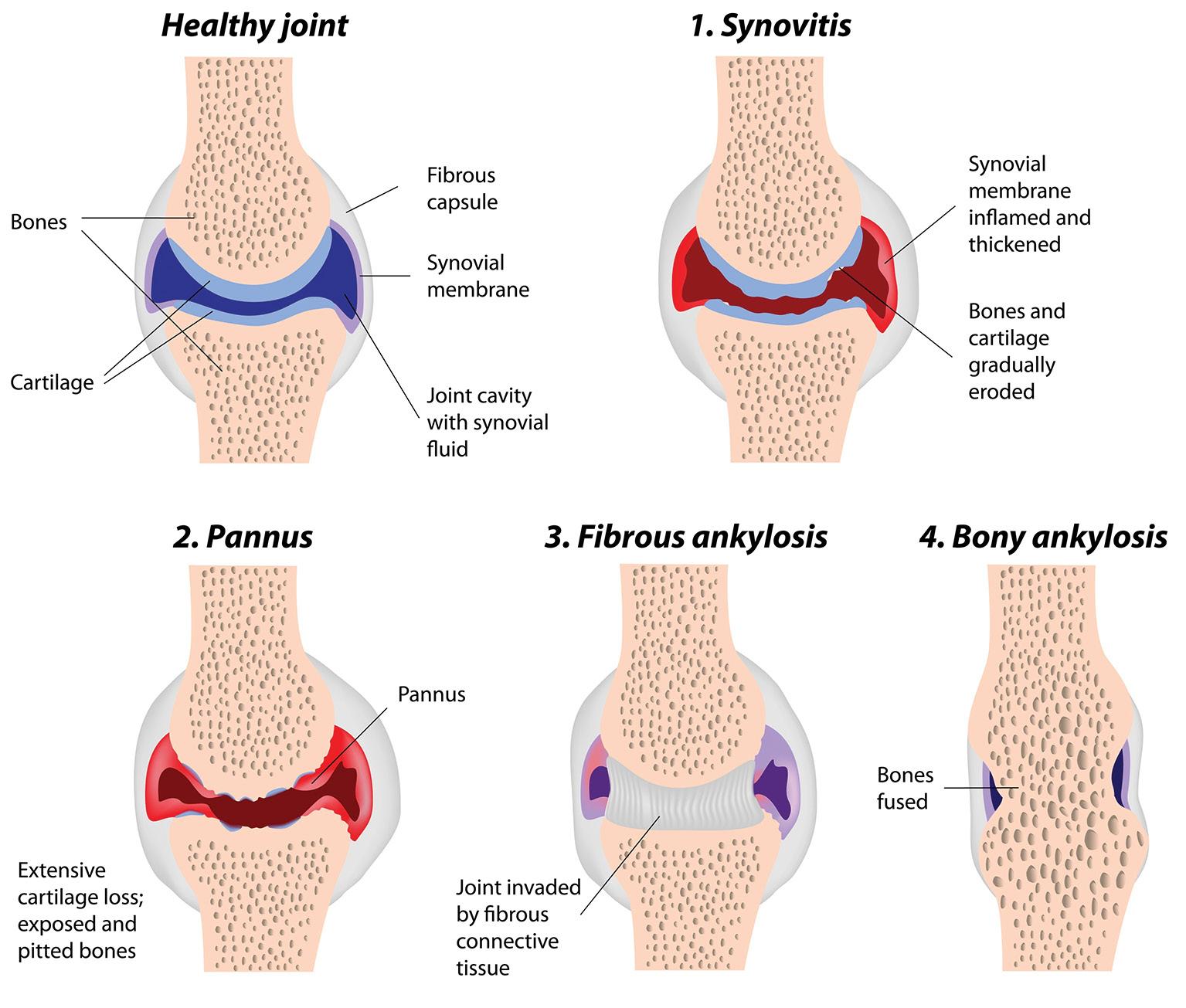
Improving access to RA care is crucial, necessitating expanded medical education for non-rheumatologists in RA diagnosis and management, stress Ford et al 12
Initiatives should start at the medical school level, extend into residency, and focus on continuing medical education for primary care practitioners. Increasing rheumatology fellowship positions can attract young physicians to the specialty and integrating mid-level providers (physician assistants and nurse practitioners) with rheumatology training into care teams can enhance patient outcomes.12
Addressing physician, patient, and systems barriers requires educating all parties about the rationale behind T2T. Redesigning care delivery and practice workflows is essential and integrating patient-reported outcomes (PROs) can play a key role.12
PROs, such as the Routine Assessment of Patient Index Data 3 (RAPID3), allow patients to report signs and symptoms, supporting T2T approaches that emphasise shared decision-making.12
Mobile health interventions, particularly smartphone applications or apps, can empower RA patients to monitor their disease activity and share information with healthcare providers. Developing apps that provide not only symptom tracking but also educational content, user security, and connectivity to healthcare providers can enhance T2T implementation.12
Learning collaboratives offer another effective approach, encouraging care teams to exchange information, test ideas, and implement successful changes. The Treatto-target in RA: Collaboration To Improve adOption and adhereNce (TRACTION) trial demonstrated the effectiveness of a learning collaborative approach in improving T2T implementation in rheumatology clinics. The TRACTION trial involved sequenced learning sessions, testing small changes in practices, and observing their effects.12
The T2T strategy has revolutionised the management of RA over the past two decades. By setting specific treatment targets, such as remission or maintaining LDA, and implementing rigorous control measures, including regular assessments and treatment adjustments, the T2T strategy has significantly improved patient outcomes.
Real-world evidence from studies indicates higher remission rates and improved QoL with T2T, supporting its effectiveness. However, challenges in implementation, including limited access to rheumatologists as well as physician and patient factors, must be addressed.
Strategies such as expanding medical education, integrating mid-level providers, and leveraging mobile health interventions can enhance T2T implementation, ultimately improving outcomes for patients living with RA.
References are available on request. SF

Osteoarthritis (OA) is one of the most prevalent chronic health conditions, affecting not only patients’ physical function but also various other aspects such as mental health, sleep, and work participation.1
OA, the most common form of arthritis, leads to multiple anatomical and physiological changes in joint tissues such as cartilage degradation, bone remodelling, and the formation of osteophytes. These changes result in clinical manifestations like pain, stiffness, swelling, and restrictions in joint function.1
About 240 million individuals worldwide are affected by OA, with 10% of men and 18% of women aged >60-years experiencing its impact. Recent data from the Global Burden of Diseases, Injuries, and Risk Factors Study reveal that the age-standardised prevalence and annual incidence rate of symptomatic, radiographically confirmed hip
and knee OA globally were 3754.2 and 181.2 per 100 000 population, respectively. These figures represent a 9.3% and 8.2% increase since 1990.1
The American College of Rheumatology (ACR) criteria for hip OA are: Pain and internal rotation <15° and flexion of the hip ≤115° or internal rotation ≥15°, pain at internal rotation, stiffness ≤60 min, and age >50-years. 2
The clinical ACR criteria for knee OA are: Pain in the knee and at least three of the following: Age >50-years, stiffness <30 min, crepitus, bony tenderness, bony enlargement and no palpable warmth. 2
A recent survey of individuals ≥20-years, showed that 29% of participants had OA in
one or more locations, including the spine, hand, hip, and knee.1
According to van Laar et al, not treating chronic OA pain is not an option. Pain relief is now considered a fundamental human right by public health organisations. Innervation and vascularisation of the articular cartilage, as well as compressive forces and hypoxia, contribute to OA pain even after inflammation subsides. 3
OA pain is characterised by both nociceptive and non-nociceptive components, including neuropathic elements arising from peripheral inflammation and central sensitisation. 3
Lifelong pain management regimens are often required. Shortterm pharmacological therapies are not effective for acute pain. Managing chronic pain in OA is challenging due to patient heterogeneity, the progressive nature of the disease, involvement of multiple pain mechanisms, comorbidities, and co-medicationespecially in frail and elderly patients. 3
Despite the plethora of analgesic options available, the risks associated with many agents create barriers in pain management, leading to undertreatment in efforts to enhance patient safety. 3
Addressing central pain mechanisms in patients living with OA requires a shift towards pain-modifying analgesic agents, according to van Laar et al. Commonly used pharmacological agents for pain control in OA include non-steroidal antiinflammatory drugs (NSAIDs), acetaminophen, opioids, and disease-modifying antirheumatic drugs, often complemented by non-pharmacological approaches. 3
The 2022 National Institute for Health and Care Excellence (NICE) guidance on the management of OA in patients >16-years, recommends topical NSAIDs for knee OA, while its use for OA affecting other joints may be considered. Topical NSAIDs are preferred over topical capsaicin, given the latter’s higher cost. 4
According to the latest Osteoarthritis Research Society International (OARSI) guidelines, high quality evidence involving a large number of patients showed modest benefits with topical NSAIDs over the course of 12 weeks. 5
Adverse events (AEs) associated with topical NSAIDs are minimal and mild. The most common AEs are local skin reactions, which were minor and transient. Topical NSAIDs are also strongly recommended for patients living with knee OA and comorbid gastrointestinal (GI) or cardiovascular (CVD) diseases and for frail patients. 5
If topical agents prove ineffective or unsuitable, an oral NSAID can be considered, considering potential drug interactions and contraindications, especially in an older population with comorbidities. 4
Caution is urged due to the potential for GI, renal, liver, and CV toxicity. Prescribing the lowest effective dose for the shortest duration is recommended, with gastroprotection, such as a proton pump inhibitor (PPI), concurrently offered. 4
The OARSI guideline also conditionally recommends oral NSAIDs for patients living with knee OA without comorbidities. The panel suggests opting for non-selective NSAIDs, preferably with the addition of a PPI, or selective cyclooxygenase-2 (COX-2) inhibitors. 5
Furthermore, the guideline recommends that for patients living with GI comorbidities, the conditional recommendation includes the use of selective COX-2 inhibitors and non-selective NSAIDs in combination with a PPI.
This recommendation is based not only on their positive effects on pain and functional outcomes but, more importantly, on their more favourable upper-GI safety profile compared to nonselective NSAIDs. 5
For patients living with CV comorbidities, the use of NSAIDs of any class is not recommended due to evidence associating NSAID use with an increased CV risk. Additionally, NSAIDs are not recommended for frail patients. 5
According to NICE, paracetamol and weak opioids are not routinely recommended but may be considered if other pharmacotherapies fail, with their use kept infrequent and for short-term pain relief. 4
Paracetamol lacks evidence for efficacy in OA pain, and weak
opioids pose potential harm without sufficient evidence supporting their efficacy. Strong opioids are discouraged for OA pain due to an unfavourable risk-benefit profile. 4
Prescribing glucosamine and other pharmacological classes, such as antiepileptics, antidepressants, rubefacients, and topical local anaesthetics, lacks substantial evidence. 4
Intra-articular corticosteroid injections are an option for shortterm relief when other pharmacotherapies are unsuccessful or to support therapeutic exercise. While evidence on their efficacy for hip OA is inconsistent, they may reduce pain in knee OA, though the effects last only two to 10 weeks. Intra-articular injection of hyaluronan is not recommended due to inconsistent benefits and potential harms, especially for hip OA. 4
Patient-initiated follow-up is encouraged, with patients advised to return if management proves inadequate. Planned follow-up is recommended under specific circumstances, such as severe symptoms, significant functional limitations, or when individuals cannot independently seek care. 4
Referral for joint replacement (hip, knee, or shoulder) should be contemplated if non-surgical management fails and joint symptoms significantly impact quality of life (QoL). The decision for referral should be based on clinical judgment rather than a numerical scoring system. 4
Factors like age, sex or gender, smoking status, co-morbidity, and body mass index (BMI) may influence surgical outcomes but should not impede the referral process. Arthroscopic lavage and debridement are not recommended. 4
PERS NALISED
Date: 17th - 19th May 2024
Venue: Elangeni Hotel, North Beach, Durban
Closing date: 20th March 2024

Beyond analgesics
The 2023 European Alliance of Associations for Rheumatology (EULAR) recommendations for the nonpharmacological management of hip and knee OA focus on comprehensive, individualised, and multi-modal approaches, reflecting the evolving understanding of the condition. 6
The recommendations reflect a shift towards a holistic and patient-centred approach to hip and knee OA management, acknowledging the importance of combining various interventions tailored to individual needs to optimise outcomes and improve the overall QoL. 6 Below is a summary of each recommendation: 6
Recommendation 1: Multicomponent management plan
Individuals with hip or knee OA should receive an individualised, multicomponent management plan that includes core nonpharmacological approaches, which include patient education, exercise, and diet, to achieve larger effects on pain and function compared to individual treatments.
Recommendation 2: Information, education, and self-management
Patients living with hip or knee OA should be provided with information, education, and advice on self-management strategies. Patient education as a single intervention shows small significant effects on pain and function in the short term, supporting the importance of reinforcing self-management strategies in subsequent clinical encounters.
Recommendation 3: Exercise programme
All individuals with hip or knee OA should be offered an exercise programme tailored to their physical function, preferences, and available services. Evidence supports the effectiveness of various exercise modalities (strength, aerobic, flexibility, neuromotor) in improving pain and function, and the choice of exercise should consider individual needs.
Recommendation 4: Mode of exercise delivery
The mode of delivery of exercises (individual or group sessions, supervised or unsupervised, face to face or digital) should be selected based on local availability and patient preferences. Technology-supported exercise and telehealth-based exercise show superior effects, emphasising the importance of aligning the delivery method with patient preferences.
Recommendation 5: Weight management
Individuals with hip or knee OA should
receive education on the importance of maintaining a healthy weight, with support for weight loss if overweight or obese. Multifocused weight loss interventions, including diet and exercise, demonstrate beneficial effects on pain and disability, and bariatric surgery is identified as the most effective pain-reducing intervention.
Recommendation 6: Assistive devices and home adaptations
Consider walking aids, appropriate footwear, assistive devices, and home adaptations to reduce pain and increase participation. Limited evidence supports the effectiveness of stable, supportive shoes, while other assistive devices may aid in daily activities and participation.
Natural products are often considered safer alternatives to pharmacology, with fewer side effects
Recommendation 7: Work-related advice
People with hip or knee OA with or at risk of work disability should receive timely advice on modifiable work-related factors. Healthcare professionals should offer guidance on factors such as working from home, assistive technology, and support from management to improve workability and participation.
Recommendation 8: Behaviour change techniques
Employ elements of behaviour change techniques when lifestyle modifications are needed (eg physical activity, weight loss). Booster sessions and combined interventions involving pain coping skills training and lifestyle behavioural weight management show positive effects on adherence to exercise and improvements in pain and function.
Do supplements have a role in OA?
Natural products are often considered safer alternatives to pharmacology, with fewer side effects. Lui et al conducted a systematic review and meta-analysis of 69 randomised controlled trials, evaluating 20 supplements for hand, hip, or knee OA.
They concluded that overall, supplements provided moderate and clinically meaningful treatment effects on pain and function.7,8
In another study by Mathieu et al, looked at the efficacy of curcumin and ginger supplementation and found that they showed significant improvement in pain and function for knee OA compared to placebo, while other treatments like NSAIDs, chondroitin, or paracetamol did not.9
Christiansen et al investigated the efficacy of avocado soybean unsaponifiables (ASU), chondroitin sulfate, hyaluronan, and glucosamine sulfate in managing mild to moderate pain and reducing NSAID use.7
ASU, derived from avocado and soybean oils, is a natural vegetable extract containing phytosterols such as β -sitosterol, campesterol, and stigmasterol. It is a complex mixture of compounds, including fat-soluble vitamins, sterols, triterpene alcohols, and potentially furan fatty acids.7
Preclinical studies demonstrate that ASUs possess chondroprotective, anabolic, and anticatabolic properties, inhibiting cartilage breakdown and promoting repair.7
ASU stimulates collagen and aggrecan synthesis by modulating inflammatory cytokines like interleukin (IL)-1, IL-6, IL8, tumour necrosis factor (TNF), and prostaglandin E2 through nuclear factorkappaB (NF-κ B) modulation.7
Clinical trials show that ASU reduces pain and stiffness while improving joint function, with efficacy observed over short to medium terms. ASU’s anti-inflammatory effects, potentially through NF-κ B inhibition, make it an anabolic agent by reducing proinflammatory mediators.7
Factors like BMI, disease severity, and activity level may influence ASU’s effect, with evidence suggesting potential protection against obesity-associated inflammatory degradation in OA. However, excessive inflammation associated with obesity may impede efficacy, similar to NSAID treatments.7
Extracts from the gum-resin of Boswellia serrata have been used in traditional medicines for centuries to address various chronic inflammatory conditions including OA. The resinous component of Boswellia serrata is rich in a diverse array of compounds, including monoterpenes, diterpenes, triterpenes, tetracyclic triterpenic acids, and notably, four major pentacyclic triterpenic acids: β - Boswellic acid, acetylβ - Boswellic acid, 11-keto- β - Boswellic acid, and acetyl-11-keto- β - Boswellic acid. These components play a crucial role in inhibiting pro-inflammatory enzymes.10
According to Ragab et al, the antiinflammatory molecular mechanism

of Boswellic acid involves the inhibition of various inflammatory factors and pathways. This includes the suppression of prostaglandins, histamine, leukotriene, and interferon- γ, along with the inhibition of 5-lipoxygenase, cytokines, TNF- α , COX-2, and inducible nitric oxide synthetase.11
Additionally, Boswellic acid has been found to upregulate free oxygen radicals and enhance antioxidant defence mechanisms mediated by catalase, glutathione peroxidase, and superoxide dismutase.11
The anti-inflammatory effects of Boswellic acid extend to the inhibition of signal transduction and transcription factors, including extracellular signal-regulated kinases 1 and 2, NF-κ B, inhibitory κ B kinase, mitogen-activated protein kinase, signal transducer and activator of transcription 3, c-Jun N-terminal kinase, SMAD2/3/4/7, and IL-1 receptor-associated kinase.11
Collectively, these multifaceted antiinflammatory mechanisms have contributed to the successful treatment of various diseases using Boswellia extracts and its phytochemicals, according to Ragab et al 11
Conditions such as OA, rheumatoid arthritis, gastric colitis, autoimmune encephalomyelitis, allergic asthma, nonalcoholic fatty liver disease, and renal fibrosis have shown positive responses to Boswellic acid-based treatments.11
The management of OA-associated pain extends beyond conventional analgesics and require a comprehensive approach that considers the multifaceted nature of the condition. Conventional pharmacological therapies, including NSAIDs, acetaminophen, and opioids, pose
challenges in managing chronic OA pain, emphasising the need for a paradigm shift towards pain-modifying analgesic agents.
The 2023 EULAR recommendations advocate for a holistic, patientcentred approach to OA management, incorporating individualised, multi-modal interventions. Non-pharmacological strategies, such as patient education, exercise, and weight management, play pivotal roles in achieving substantial pain relief and functional improvement.
The 2023 EULAR recommendations advocate a holistic, patient-centred approach to OA management
Additionally, natural products like ASU and Boswellia serrata extracts are promising alternatives, demonstrating anti-inflammatory effects and symptommodifying properties.
The integration of these diverse approaches holds the potential to revolutionise OA treatment, providing safer and more effective options beyond traditional analgesics. The shift towards a holistic perspective on pain management emphasises the importance of tailoring interventions to individual needs, optimising
Kellgren and Lawrence criteria for assessment stage of osteoarthritis. The classifications are based on osteophyte formation and joint space narrowing.

outcomes, and improving overall quality of life for individuals living with OA.
1. Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis and Cartilage, 2022.
2. Schiphof D, Runhaar J, Waarsing EJ, et al The 10-year course of the clinical American college of rheumatology (ACR) criteria for hip and knee osteoarthritis in an early symptomatic cohort, data from check. Osteoarthritis and Cartilage, 2018.
3. van Laar M, Pergolizzi JV Jr, Mellinghoff HU, et al Pain treatment in arthritis-related pain: beyond NSAIDs. Open Rheumatol J, 2012.
4. National Institute for Health and Care Excellence. Osteoarthritis in over 16s: diagnosis and management. NG226. October 2022. Available from: https://www.nice.org.uk/guidance/ng226
5. Bannuru RR, Osani MC, Vaysbrot EE, et al OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage, 2019.
6. Moseng T, Vlieland TMV, Battista S, et al EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis: 2023 update. Annals of Rheumatic Diseases, 2023.
7. Christiansen BA, Bhatti S, Goudarzi R, Emami S. Management of Osteoarthritis with Avocado/ Soybean Unsaponifiables. Cartilage, 2015.
8. Liu X, Machado GC, Eyles JP, Ravi V, Hunter DJ. Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. Br J Sports Med, 2018.
9. Mathieu S, Soubrier M, Peirs C, et al A MetaAnalysis of the Impact of Nutritional Supplementation on Osteoarthritis Symptoms. Nutrients, 2022.
10. Pawar RK, Sharma S, Singh KC, Sharma RK. Physico-chemical standardization and development of HPTLC method for the determination of β -boswellic acid from Boswellia serrata Roxb (exudate). Int J App Pharm, 2011.
11. Ragab EA, Abd El-Wahab MF, Doghish AS, et al. The journey of Boswellic acids from synthesis to pharmacological activities. NaunynSchmiedeberg’s Arch Pharmacol, 2024.
12. iNova Pharmaceuticals. New supplement launched to reduce symptoms of osteoarthritis. 2023. [Internet]. Available at: https://medpharm.co.za/ home-featured/new-supplement-launched-toreduce-symptoms-of-osteoarthritis/
13. Professional Information. Posteon. 2022. [Internet]. Available at: https://inovapharma.co.za/wpcontent/uploads/2022/10/Posteon-PI.pdf SF


Glaucoma, the second leading cause of blindness globally, is characterised by progressive degeneration of the optic nerve, resulting in the loss of retinal ganglion cells, thinning of the retinal nerve fibre layer, and increased excavation of the optic disc.
Glaucoma is divided into openangle and closed-angle types, further classified as primary or secondary based on contributing factors. About 80 million people are affected worldwide, with a projected increase to around 111 million by 2040, with the highest incidence of primary open-angle glaucoma observed in African countries.
Open-angle glaucoma, more prevalent with age, affects 0.4% at 40-44 years and increases to 2.7% at 70-74 years, with a higher risk in men and individuals of African descent.
Unfortunately, it often remains asymptomatic until advanced stages, leading to delayed diagnosis. In contrast, closed-angle glaucoma presents with acute symptoms, including eye pain, visual impairment, and nausea, requiring immediate intervention to prevent severe damage and blindness.
The impact of glaucoma on the quality of life is substantial, as it leads to irreversible visual field defects, affecting peripheral, central, and paracentral areas.
Patients experience difficulties in daily activities, leading to an increased risk of accidents and, in advanced stages, complete blindness. Glaucoma also impairs contrast sensitivity and dark adaptation, further hindering activities such as nighttime driving.
Additionally, the adverse effects of treatment, emotional challenges, and financial burdens contribute to negative emotions like anxiety and depression.
Various risk factors, including age, ethnicity, elevated intraocular pressure (IOP), high myopia, and a positive family history of glaucoma, influence its development.
Studies suggest that reducing IOP by 22.5% can significantly lower the five-year risk of developing open-angle glaucoma. However, diagnostic delays are common due to the asymptomatic nature of openangle glaucoma, with around 40% of retinal nerve fibres lost by the time defects are noticed. Regular screenings from age 40 and tonometry are recommended for early detection.
The term glaucoma is derived from the Greek word glaukós, a non-specific term for green or light grey
The diagnosis involves funduscopic examination, measuring IOP, and morphometric techniques using optical coherence tomography (OCT) for quantitative assessment.
Glaucomatous changes include tissue loss at the neuroretinal rim, optic nerve excavation enlargement, haemorrhages, thinning of the retinal nerve fibre layer, and
parapapillary tissue atrophy. Monitoring disease progression is essential, and new imaging procedures offer more precise assessments.
Preventing glaucoma progression primarily focuses on reducing IOP through treatments like eyedrops, laser therapy, and surgery. Eyedrops, particularly prostaglandin analogues, are commonly prescribed, with preservative-free options developed to improve tolerance.
Laser therapy, such as trabeculoplasty and cyclophotocoagulation, may be considered if local treatment is insufficient. Surgical interventions include minimally invasive, filtering, and non-filtering procedures, each with varying side effects and efficacy. Regular monitoring of IOP is crucial, and adjustments to the target pressure may be necessary based on ongoing evaluations.
Glaucoma encompasses a spectrum of disorders with progressive optic nerve degeneration. As the global prevalence continues to rise, understanding the distinctions between open and closed angle glaucoma becomes crucial. The impact on QoL, combined with challenges in early diagnosis and treatment, emphasises the need for effective prevention and intervention strategies. Early diagnosis, lowering IOP, and personalised interventions remain key in the ongoing battle against glaucoma-induced blindness.
Please note, this is just a summary of the article. To read the full article, go to www.medicalacademic.co.za. SF

Hearing loss is one of the most common chronic conditions experienced by older adults, with a prevalence of ~50% in those >75-years and data show hearing loss is increasing in younger people. Globally, >80% of ear and hearing care needs go unmet.1,2
According to the World Health Organization, changing mindsets about the importance of ear and hearing care is essential to enhance accessibility, and reduce the economic burden (around US$1trillion annually) associated with unaddressed hearing loss.1
Hearing loss has profound impact on individual’s ability to connect, share ideas, and participate fully in daily activities. The importance of treating hearing loss is underscored by its impact on communication, social engagement, and overall well-being, writes Wallhagen.2
However, despite the functional and psychosocial significance of hearing, a mere 20% of those who could benefit from hearing aids actually use them, with various reasons contributing to this gap, such as cost, perceived lack of benefit, and, notably, the
persistent stigma associated with hearing loss and hearing aid use.2
Stigma emerges as a multifaceted barrier throughout the experiential continuum of hearing loss. It affects initial acceptance, decisions to seek testing or treatment, the choice of hearing aids, and even when and where these aids are worn. The perceived stigma is deeply intertwined with three interrelated experiences: Changes in selfperception, ageism, and vanity.2
Changes in self-perception involve individuals grappling with the meaning of hearing loss, often contrasting feelings of wholeness with a sense of disability or cognitive impairment.
Some patients engage in behaviours like ‘faking’ hearing to avoid admitting their condition, contributing to delays in acknowledgment and treatment. The societal context in which these individuals grew up influences how they perceive hearing loss, with historical stigmas contributing to their hesitation in openly accepting it.2
Ageism plays a significant role. The fear of being labelled as ‘old’ or ‘disabled’ leads individuals to resist using hearing aids, as these devices symbolise an acknowledgment of ageing and associated limitations. This perception is reinforced by societal norms, where youth is valued, and physical disabilities are sometimes recoiled from.2
Vanity further complicates matters, as individuals express concerns about the appearance of hearing aids. The desire to hide these devices stems from a fear of being perceived as unattractive or old. Vanity influences decisions to seek treatment, contributing to a delay in addressing hearing loss. 2
Interestingly, not all individuals are equally affected by perceived stigma. Some reject its importance outright, emphasising the necessity of ‘getting over it’. This resilience might stem from a combination of factors, including age-related changes in perspective and a prioritisation of improved hearing over societal judgments.2
Role players who perpetuate stigmas The media and advertising as well as some healthcare professionals play a role in perpetuating stigmas. Advertisements often emphasise the invisibility of hearing aids, reflecting a societal bias against visible aids, according to Wallhagen. 2
Healthcare providers sometimes dismiss the importance of hearing loss or associate it solely with ageing, reinforcing existing stigmas. The influence of supportive or non-supportive communication partners is crucial. Partners who view hearing aids negatively may unintentionally discourage seeking treatment. 2
The dynamics of relationships, where discussing hearing loss is often considered ‘taboo’, can lead to a lack of open communication about treatment options. 2
How can hearing loss stigma be addressed?
Ultimately, states Wallhagen, addressing the stigma associated with hearing loss requires a comprehensive approach. She recommends that initiatives should focus on reshaping societal perceptions, challenging ageism, and promoting positive representations of hearing aids. 2
Additionally, fostering open communication within relationships and providing support networks can empower individuals to overcome the barriers posed by stigma, ultimately improving access to hearing care and enhancing overall well-being.2
Sensorineural hearing loss: The most prevalent form of hearing impairment that can arise from various factors such as ageing, prolonged exposure to loud noise, injury (eg a head injury that affect the auditory system), diseases (eg acoustic neuroma, otosclerosis, Ménière’s disease, hypertension), certain medications (eg aminoglycoside antibiotics, large amounts of aspirin, loop diuretics, and some chemotherapy agents), or genetic predisposition. Typically not amenable to medical or surgical interventions, individuals with sensorineural loss often benefit from hearing aids.3,4
Conductive hearing loss: Occurs in the outer or middle ear, where sound waves face obstruction before reaching the inner ear. Causes may include earwax blockage, foreign objects in the ear canal, fluid accumulation, infections, or structural abnormalities. In certain cases, medical or surgical interventions can reverse conductive hearing loss. Children, especially those with recurrent ear infections or a tendency to insert foreign objects, commonly experience this type.3
Mixed hearing loss: Some individuals may
exhibit a combination of both sensorineural and conductive hearing loss. Initially having sensorineural impairment, they may later develop a conductive component. Hearing testing is crucial for determining the specific type of hearing loss, guiding appropriate care solutions. Hearing aids offer effective options, and alternative interventions beyond hearing aids are also accessible.3
It is essential to consider depression and dementia as potential contributing factors to hearing loss. Apathy, inattentiveness, and social disengagement, which are common manifestations of hearing loss, can also be indicative of both depression and dementia.5
Evaluating patients for hearing impairment is crucial in cases of dementia, as untreated hearing loss may exacerbate disengagement and potentially exaggerate the perceived severity of cognitive impairment.5
Likewise, when hearing loss is identified, it is advisable to conduct cognitive screening, as cognitive impairment frequently coexists with hearing loss. This reciprocal consideration helps ensure a comprehensive approach to addressing both auditory and cognitive aspects of a patient’s health.5
The management of hearing loss in primary care involves a collaborative approach between general practitioners and audiologists. While audiologists often handle the treatment of hearing aids, general practitioners play a crucial role in addressing specific aspects of hearing loss.5
The SCREAM mnemonic (Sudden sensorineural hearing loss, Cerumen impaction, Auditory rehabilitation, Education, Assistive devices, and Medications) provides a concise framework for general practitioners to consider when managing hearing loss.5
Sudden sensorineural hearing loss is characterised by a rapid decline in hearing over a short period without an identifiable cause. General practitioners should promptly confirm hearing loss through audiometry and refer the patient to an otolaryngologist within one week for further evaluation.5
While the use of glucocorticoids for idiopathic sudden sensorineural hearing loss remains inconclusive, some studies suggest benefits from systemic or intratympanic steroids.5
Cerumen impaction, resulting in conductive hearing loss, can be effectively treated by general practitioners through methods such as irrigation, manual extraction, or cerumenolytic agents (liquid solutions that help thin, soften, break up, and/or dissolve ear wax).5
Despite limited evidence favouring one removal method over others, irrigation is
often preferred in primary care due to its minimal training requirements and favourable side effects.5
Auditory rehabilitation involves assisting patients and their families in adapting to hearing deficits and improving communication strategies. Although studies supporting auditory rehabilitation are of varying quality, practices such as facing individuals when talking, optimising lighting, and minimising background noise are generally regarded as beneficial.5
Education is a key component of hearing loss management. Patients should be provided with information about the nature and causes of hearing loss, hearing aids, and hearing protection.5
Assistive devices, including hearing assistive devices and direct-to-consumer hearing aids (mild hearing loss), can be recommended by general practitioners to address communication challenges. Awareness of available hearing technologies and their appropriateness for individual patients is essential.5
Medications associated with ototoxicity should be carefully monitored, considering factors such as dose dependence and increased risk in patients with heart failure and chronic kidney disease.5
World Hearing Day 2024 highlights the urgent need to address the misperceptions and stigmas surrounding hearing loss. Addressing stigma requires comprehensive initiatives focusing on challenging ageism, promoting positive representations of hearing aids, and fostering open communication.
Understanding the diverse types of hearing loss, including sensorineural, conductive, and mixed, is fundamental for effective management. The SCREAM mnemonic provides a concise framework for general practitioners, emphasising prompt evaluation of sudden sensorineural hearing loss, effective treatment of cerumen impaction, and comprehensive approaches to auditory rehabilitation, education, and assistive devices.
The impact of hearing loss extends beyond audiological considerations, with implications for mental health, cognitive function, and social engagement. Recognising the interplay between hearing loss, depression, and dementia underscores the importance of holistic patient care.
Collaboration between general practitioners and audiologists ensures a comprehensive approach, addressing both auditory and cognitive aspects of a patient’s health.
References are available on request.

Consuming an excessive amount of sodium is associated with elevated blood pressure (BP), which increases the risk of stroke, cardiovascular (CVD) and renal diseases. One of the challenges, however, is that there is still no clarity of what constitutes too much sodium.1,2
Salt is one of the main sources of sodium (comprises ~40% sodium and 60% chloride, see Table 1). Chloride is a mineral found naturally in various foods. It plays a crucial role in regulating the movement of fluids and various nutrients across cell membranes. 3,4
World Health Organization (WHO) data show that around two million deaths can be linked to a high salt diet annually. Global salt intakes average 10.8g/day, more than double the recommended limit for adults. According to the WHO implementing effective salt reduction policies to reduce global intake by 23% by 2030 can reduce deaths from CVD by 3%. 2
The American Food and Drug Administration points out that the terms sodium and salt are frequently used
interchangeably but in fact have different meanings. Dietary salt is a crystalline
Iodised
Kosher salt, coarse
Kosher salt, fine 1120mg
Sea salt, fine 2120mg
Sea salt, coarse 1560mg
Pink (Himalayan) salt 2200mg
Black salt 1150mg-2200mg
Fleur de sel (salt that forms as a thin, delicate crust on the surface of seawater as it evaporates) 1560mg-2320mg
Potassium salt
compound found abundantly in nature, while sodium is a mineral and a chemical element of salt. 4
Sodium is an essential nutrient needed by the body in relatively small amounts (provided that substantial sweating does not occur) to maintain a balance of body fluids and keep muscles and nerves running smoothly. 4
Sodium has various culinary purposes, such as curing meat, aiding in baking, thickening, preserving moisture, and intensifying flavour (including that of other ingredients). 4
Furthermore, certain common food additives like monosodium glutamate (MSG), sodium bicarbonate (baking soda), sodium nitrite, and sodium benzoate contain sodium, albeit in smaller quantities, contribute to overall sodium content. 4
The American Heart Association notes that ~75% of sodium intake is attributed to

processed and restaurant foods. According to the Vital Signs report drafted by the American Centres for Disease Control and Prevention (CDC), >40% of sodium consumption can be linked to 10 specific food categories. 6,7
These include common items like breads, luncheon meats (such as deli ham or turkey), pizza, poultry, soups, cheeseburgers, sandwiches, cheese, pasta dishes, meat dishes, and snack foods like potato chips, pretzels, and popcorn (see Table 2).7
Sodium plays a pivotal role in BP regulation. Each individual responds differently, leading to the concept of salt-sensitive and salt-resistant BP. Salt-sensitive BP is characterised by elevated BP linked to high salt intake. About 50% of individuals with hypertension have salt sensitivity,
a percentage that fluctuates based on gender and is also influenced by racial factors. Among those with normal BP, around 26% display salt sensitivity, contributing to heightened mortality rates. Salt-resistant simply means intake has no effect on the individual, which may explain why not all obese patients have hypertension. 8,9
The physiological mechanisms underlying salt-sensitive BP involve interactions within renal function, fluid hormones, vasculature, the heart, and central sympathetic outflow, often influenced by genetic factors. 8
Studies have established that sodium loading induces extracellular volume expansion and volume-loaded hypertension, emphasising the role of the kidneys in salt sensitivity. 8
Beyond BP elevation, increased dietary sodium can adversely affect various target organs independently of BP changes.
Arteries may experience impaired endothelial function and increased stiffness due to sodium, impacting CV health. 8
Sodium loading is associated with increased left ventricular mass, and kidney function may decline with high sodium, affecting proteinuria and albuminuria. The brain’s autonomic control of BP is influenced by sodium, potentially leading to increased sympathetic outflow, even without elevated average BP. 8
Meta-analyses demonstrate a strong association between sodium intake and systolic BP (SBP), with sodium restriction showing a reduction in SBP, particularly in older age, among black populations, and hypertensive patients. 8
A recent study by Gupta et al examined individuals’ BP responses to dietary sodium, assessed the differences in BP among individuals randomised to either a high(~2200mg sodium added daily to usual
Food group
Baking soda, baking powder
Bouillon cubes, powdered broths, soups, gravies
Soy sauce
38 000mg
20 000mg
7000mg
Snack foods (eg pretzels, cheese puffs, popcorn) 1500mg
Potato chips (28gr) 147mg
Bacon 1500mg
Sauces and spreads 1200mg
Cheese, hard 800mg
Processed vegetables 600mg
Butter/margarine 500mg
Cheese, soft 400mg
Processed fish 400mg
Cereals and cereal products (eg bread, breakfast cereals, biscuits, cakes, pastries) 250mg
Fish, raw or frozen 100mg
Eggs 80mg
Milk and cream 50mg
Vegetables, fresh or frozen 10mg
Fruits, fresh or frozen 5mg
Corned beef, canned 950mg
Bran (flakes) 1000mg
Cheese (hard cheese, average) 620mg
Cheese (processed) 1320mg
Fish fingers, fried in blended oil 350mg
Peanuts (roasted and salted) 400mg
Potato chips (homemade, fried in blended oil) 12mg
Oven chips (baked) 53mg
Tuna in brine 320mg
Pizza slice 598mg
Kentucky Fried Chicken (one breast)
1080mg
Kentucky (one drumstick) 360mg
McDonald’s cheeseburger 643mg
Canned soup
Pasta (250 gr)
360mg-800mg
412mg-1887mg
diet) or low-sodium (~500mg) diet first, and investigated potential variations based on baseline BP levels and the use of antihypertensive medications.10
Around 25% of participants were normotension, 20% had controlled hypertension, 31% had uncontrolled hypertension (31%), and 25% had untreated hypertension.10
When consuming their usual, highsodium, and low-sodium diets, participants had median SBP measures of 125mmHg, 126mmHg, and 119mmHg, respectively.10
The median within-individual change in mean arterial pressure between high- and low-sodium diets was 4mmHg, and this change did not significantly differ based on hypertension status. In comparison to the high-sodium diet, the low-sodium diet led to a decrease in mean arterial pressure in 73.4% of individuals.10
Using the commonly employed threshold of a 5mmHg or greater decline in mean arterial pressure between high- and lowsodium diets classified 46% of individuals as salt-sensitive.10
At the conclusion of the first week of dietary intervention, the mean SBP difference between individuals assigned to a high-sodium versus a low-sodium diet was 8mmHg. This difference was consistent across subgroups defined by age, sex, race, hypertension, baseline BP, diabetes, and body mass index.10
Okay, so we know too much sodium is bad. However, there is some controversy surrounding the definition of what constitutes ‘excess’ sodium intake.1,2
The average individual consumes >4310mg sodium every day, which equates to 10.78g of salt per day. To reduce sodium intake, the WHO guideline recommends a maximum of <2000mg sodium a day (<5g/day salt) to reduce the risk of CVD and stroke.11
For children (aged two- to 15-years, the WHO recommends adjusting the adult dose ‘downward’ based on their energy requirements. This recommendation for children does not address the period of exclusive breastfeeding (<6-months) or complementary feeding with continued breastfeeding (six- to 24-months).11
How were these values determined?
According to Mente et al, there is currently no compelling evidence supporting the sustainability of such low sodium levels (<2000mg sodium a day) or demonstrating consistent links between low sodium intake and reduced CV risks.12
Current guidelines primarily rely on shortterm intervention trials linking sodium intake with BP. However, evidence from cohort studies reveals a J-shaped relationship between sodium intake and CV events, suggesting that the lowest risk occurs within the range of 3g/day to 5g/day.12
Study results are inconsistent, according to Mente et al. While observational
studies, such as International Cooperative Study on Salt, Other Factors, and Blood Pressure, have shown positive associations between sodium intake and BP, findings from cohort studies, like the Prospective Urban Rural Epidemiology (PURE) study, highlight a threshold association, indicating increased CV risks at both high and low sodium intakes.12
Randomised controlled trials, notably the Dietary Approaches to Stop HypertensionSodium Intake and Blood Pressure trial, have influenced recommendations for lower sodium intake, but their short durations and controlled settings raise questions about real-world applicability, state Mente et al 12
Furthermore, evidence reveals the near-impossibility of achieving and sustaining a very low sodium intake, even with intensive dietary counselling, as demonstrated by studies such as the Trials of Hypertension Prevention -II. The challenge lies in the inherent difficulties of maintaining such dietary restrictions over an extended period.12
Despite meta-analyses suggesting a potential reduction in CV disease with sodium lowering, these analyses are inconclusive and lack specific emphasis on the recommended target of low sodium intake (<2000mg sodium a day). The WHO does state that reducing salt intake is the most viable option to reduce sodium intake.11,12
Reducing sodium intake presents a pivotal opportunity for cardiovascular health, with the WHO advocating for a 23% global salt reduction by 2030, potentially preventing millions of deaths. However, the ongoing debate about defining excessive sodium intake highlights the complexity of establishing universal guidelines. While studies link sodium reduction to decreased BP and CV risk, sustaining very low sodium levels proves challenging in the real-world setting. The controversy underscores the need for comprehensive research, emphasising practicality, longterm impacts, and individual variability in sodium-related health outcomes.
References are available on request. SF












Moderate-severe pancreatitis is characterised by
described as acute inflammation of the pancreas, usually
abdominal pain and elevations of serum pancreatic enzymes. AP accounts
hospital admissions for pancreatic disease and
been described as one of the most unpredictable diseases of the digestive system.1,2,3
Severe pancreatitis is defined by the presence of local complications combined with persistent organ failure.
Severe pancreatitis affects a ~15%-20% of patients. 3
Cholelithiasis (gall stones) and excessive alcohol intake are the leading risk factors, which collectively are responsible for >60% of cases.4 About 60% of patients require admission to intensive care units (ICUs) within the initial days of the disease due to an intense systemic inflammatory syndrome response resulting in pancreatic tissue and/or peri-pancreatic tissue necrosis. In about 30% of patients, infection of the peri-pancreatic necrosis occurs, which is associated with mortality rates varying from 15% to 39%. 2,3,4
About 50% of AP-related deaths occur within the initial two weeks of the disease, primarily due to multiple organ failure. The remaining fatalities occur later due to complications arising from peri-pancreatic necrosis and subsequent interventions. 3
About 80% of patients have mild symptoms that can be treated with supportive therapy involving fluids, pain relief, and resumption of a normal diet. Recommendations for supportive treatment include:2
_ Moderate fluid resuscitation (10ml/kg bolus in case of hypovolaemia, followed by 1.5ml/kg/h) using Ringers lactate
_ An on-demand diet as soon as tolerated. Consider feeding tube placement if diet has not been resumed after three days
_ A multimodal approach to pain management that includes paracetamol, metamizole and simple opiates. When insufficient consider epidural analgesia
_ Prophylactic antibiotics, pre, pro, and postbiotics are not currently recommended.
Efficient management necessitates accurate diagnosis and treatment by a multi-disciplinary team including specialised surgeons, gastroenterologists, intensivists, and radiologists. This multi-disciplinary approach aims to reduce both morbidity and mortality rates. In recent decades, the treatment paradigm has shifted from aggressive open surgery towards a more conservative strategy, incorporating minimally invasive techniques.
Despite improvements in recent treatment approaches, infected peri-pancreatic necrosis remains challenging to manage, according to van den Berg and Boermeester. 2
Besides supportive care until the inflammation resides, no specific therapies are yet available to mitigate or prevent (peri-) pancreatic necrosis. Supportive care recommendations include:2
_ Carbapemens is the first choice of antibiotics for treatment of infected necrosis, although robust evidence is lacking
_ Procalcitonin may be used as guidance when antibiotic therapy is considered to reduce unnecessary antibiotic use _ Drainage of infected necrotic collections should be delayed and treated with antibiotics alone if possible
_ Modality of drainage (percutaneous, trans-gastric plastic of lumen-apposing metal stents) should be discussed interdisciplinary and depends on the location and extent of the collections, and local availability and expertise
_ Neostigmine treatment should be considered for patients admitted to the ICU with intra-abdominal hypertension
_ Patients with biliary necrotising pancreatitis should be closely monitored following discharge and offered cholecystectomy when collections have been resolved
_ Extracorporeal cytokine removal might be considered as a last resort for persistent organ failure in selected cases.
References are available on request. SF




WHO adds cladribine, glatiramer acetate and rituximab to the MS EML
The earliest known documentation of multiple sclerosis (MS) dates back to the case of Lidwina the Virgin in 1395, who experienced symptoms such as blindness, weakness, and pain after a fall while skating.
Today, MS is a progressive autoimmune disease affecting around 2.8 million people globally, with prevalence in Africa potentially underestimated due to challenges like underreporting. Specific alleles and factors like Epstein-Barr virus, vitamin D deficiency, smoking, and obesity contribute to MS risks in African populations.
Managing MS in Africa poses challenges including lack of awareness, limited access to healthcare, financial constraints, and socio-cultural factors leading to delayed diagnosis and treatment. Patients face difficulties in testing accessibility, social isolation, and discrimination, exacerbated by the lack of support groups.
The signs and symptoms of MS include fatigue, muscle weakness, pain, visual disturbances, and cognitive dysfunction. As MS progresses, patients may become increasingly disabled, impacting mobility, self-care, and independence. The disease also affects various aspects of life, leading to unemployment, strain on family dynamics, and financial burden.
Cognitive dysfunction, fatigue, and
depression are often overlooked by healthcare professionals. Depression, prevalent in up to 50% of MS patients, significantly affects quality of life, with suicidal rates twice as high as the general population. Anxiety and stress levels are high due to uncertainties about the disease’s course and its impact on daily life.
MS is classified into relapsing-remitting, secondary progressive, primary progressive, and progressive-relapsing types. Diseasemodifying therapy (DMT) is the mainstay treatment, targeting the immune system to prevent relapses, slow disease progression, and alleviate symptoms.
The Middle East North Africa Committee for Treatment and Research in Multiple Sclerosis updated their treatment algorithm in 2023, incorporating new medications listed by the World Health Organization (WHO) in the Model Lists of Essential Medicines. The WHO’s decision to include cladribine, glatiramer acetate, and rituximab in the Essential Medicines List aims to improve global access to MS treatment. Off-label use of rituximab is supported by evidence of efficacy and
safety, potentially providing major health benefits worldwide.
In conclusion, while MS has historical roots dating back centuries, the contemporary landscape reveals challenges in managing the disease in Africa. Awareness, access to healthcare, and socio-cultural factors contribute to the difficulties faced by MS patients. The impact extends beyond physical symptoms, affecting mental health and overall quality of life. Advances in treatment options and global initiatives aim to address these challenges and improve outcomes for individuals living with MS.
Please note, this is just a summary of the article. To read the full article, go to www.medicalacademic.co.za. SF

TTesticular cancer (TCa) predominantly affects younger males aged between 15- to 40-years, and its survival rates are relatively high, reaching 99% for localised disease.
he global incidence of TCa, as reported by the International Agency for Research on Cancer in 2020, was 74 458 cases, with significant variation across regions.
In Africa, there is a lower reported prevalence, possibly due to underreporting, but mortality rates are higher, indicating challenges in resource availability and advanced stage diagnoses.
In South Africa, cancer incidence statistics reveal that TCa accounts for ~10% of malignancies in males aged between 20- and 39-years. Cryptorchidism (undescended testis), genetic factors, and

environmental influences contribute to TCa risk.
Cryptorchidism increases the risk by 3.7-7.5 times, with Klinefelter syndrome being a common cause. Genetic studies have identified several loci associated with TCa, and environmental risk factors include viral infections, testicular trauma, exposure to certain chemicals, and physical factors like heat stress.
Testicular germ cell tumours (TGCT) represent 90%-95% of TCa cases, with seminomas and non-seminomas being the main histological types. Grobler et al’s study in South Africa indicates a higher five-year survival rate for seminomas (91%) compared to nonseminomas (78%). Unfortunately, the majority of African patients are diagnosed at stage 3, impacting survival rates.
Common signs of TCa include painless testicular masses, and metastasis may lead to various symptoms such as nausea, vomiting, abdominal pain, and back pain.





Diagnosis involves medical assessment, physical examination, and testicular ultrasound, while further evaluation includes serum tumour markers and imaging. Treatment often involves surgical removal of the affected testicle, followed by additional interventions based on disease stage and response. Factors influencing metastatic relapse vary by histological type, with primary tumour size and stromal invasion predicting relapse in seminomas.
Lymphovascular invasion (LVI) is a key predictor for nonseminomas, with a higher risk of relapse at five years for cases with LVI compared to those without. Salvage chemotherapy is a standard approach for relapsed or refractory disease, and late relapses may involve surgery or salvage chemotherapy based on resectability.
Patients with progressing tumours following initial chemotherapy may be candidates for high-dose chemotherapy or peripheral blood stem cell transplantation. Both approaches show promising progression-free and overall survival rates.
TCa presents unique challenges, particularly in the African context, with potential underreporting and late-stage diagnoses contributing to higher mortality rates. Cryptorchidism and genetic factors play significant roles in TCa risk, and effective management involves a combination of surgical interventions and chemotherapy, tailored to disease stage and response. Early detection and comprehensive treatment strategies are essential for optimising outcomes in testicular cancer patients.
Please note, this is just a summary of the article. To read the full article, go to www.medicalacademic.co.za. SF







When anxiety
and
stress creep in IBS symptoms flare up
1

clinic referrals 2
• In patients with IBS, the gut microbiome is associated with psychological distress, anxiety and depression 2

• IBS is caused by a disruption in the gut-brain axis (BGA) 3
• Neurotransmitters play an important role in regulating the microbiota-gut-brain axis 3
• Dysregulation of the gut microbiota plays a role
2
Relieving the spasm and stress of IBS is a simple 2-in-1 tablet taken 2-4 times daily Librax®, the 2-in-1 treatment for stress-related IBS, combines the anti-anxiety action of chlordiazepoxide and the antispasmodic effects of clinium bromide.
*IBS - Irritable Bowel Syndrome
Bowel Syndrome and the Gut Microbiome: A Comprehensive Review. J Clin Med 2023;12(7):2558. 3. Chen M, Ruan G, Chen L, Ying S, Li G, Xu F, et al. Neurotransmitter and Intestinal Interactions: Focus on the Microbiota-Gut-Brain Axis in Irritable Bowel Syndrome. Front Endocrinol (Lausanne). 2022;13:817100.